Neobladder reconstruction
Overview
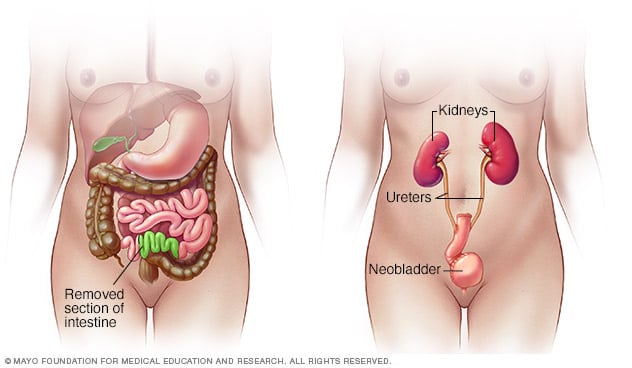
Neobladder reconstruction is a surgical procedure to construct a new bladder.
If a bladder is no longer working properly or is removed to treat another condition, a surgeon can create a new way for urine to exit the body (urinary diversion). Neobladder reconstruction is one option for urinary diversion.
During the procedure, a surgeon uses a piece of intestine to create a new bladder. The new bladder allows a person to urinate voluntarily and control when to urinate.
The procedure is also called an orthotopic neobladder reconstruction. Orthotopic refers to things being in their usual place in the body. The new bladder is placed in the same location as the original bladder.
Why it's done
Neobladder reconstruction is an option when a bladder is surgically removed because it is diseased or no longer works properly. Some reasons that people have their bladders removed include:
- Bladder cancer
- A bladder that no longer works properly, which can be caused by radiation therapy, neurological conditions, chronic inflammatory disease or other disease
- Urinary incontinence that hasn't responded to other treatment
- Conditions present at birth that cannot be repaired
- Trauma to the bladder
Risks
Several complications may occur with neobladder reconstruction, including:
- Bleeding
- Blood clots
- Infection
- Urine leaks
- Urine retention
- Electrolyte imbalances
- Vitamin B-12 deficiency
- Loss of bladder control (incontinence)
- Cancer of the intestine
How you prepare
Food and medications
Your surgeon may ask you to have a clear liquid diet for 1 to 2 days before surgery. You'll likely need to stop eating and drinking after midnight on the night before your procedure. Let your doctor know about all of the medications, vitamins and dietary supplements you're taking. In some cases, you may need to stop these medications before your surgery.
Learning to self-catheterize
Being unable to empty the bladder completely (urinary retention) is a potential complication of neobladder reconstruction. If this happens, you need to be willing to do self-catheterization. In self-catheterization, you put a narrow tube (catheter) through the opening to your bladder (urethra) to drain urine and relieve pressure on the bladder. A nurse or other health care provider will teach you how to self-catheterize.
What you can expect
Before the procedure
Your surgeon orders tests to check your kidney function and to make sure that you don't have a urinary tract infection. You may also have an imaging test, such as a CT scan, of your urinary tract to check the ureters — tubes that carry urine from the kidneys to the bladder — to see that they are in good condition.
During the procedure
The general steps in neobladder reconstruction include:
- Removing the nonfunctioning or diseased bladder
- Separating a portion of the large intestine, small intestine or parts of both
- Reshaping intestinal tissue into a spherical bladder
- Placing the new bladder in the same location as the original bladder
- Attaching the new bladder to the ureters
- Attaching the new bladder to the tube that controls the release of urine from the body (urethra)
- Repairing the intestines
- Placing a temporary catheter in the urethra for draining the bladder during recovery
Your surgeon may perform the procedure through a single opening in your abdomen or with a laparoscopic approach. Laparoscopic surgery involves several very small openings for imaging and surgical tools to pass into the lower abdomen. This surgery may also be performed with the use of robotic devices.
After the procedure
The hospital stay after neobladder reconstruction is usually about 3 to 5 days.
Before you leave the hospital, a nurse or other health care provider will give you written instructions and talk to you about the following:
- Wound care
- Catheter management
- A regular schedule for draining your bladder
- Exercises to strengthen the pelvic floor
- Follow-up appointments for monitoring recovery and how well the new bladder is working
It may take some time for the neobladder to work well. Immediately after surgery, you may have a difficult time controlling your bladder and may experience involuntary loss of urine (urinary incontinence). This may happen until the neobladder stretches to a typical size and the muscles that support it get stronger.
Daytime bladder control (continence) usually improves over the first 6 to 12 months after surgery. Nighttime continence may continue to improve through the second year. Persistent problems with incontinence are more common during the night.
Lifelong follow-up is needed after a neobladder reconstruction. Ask your doctor how often you should plan to return for follow-up visits.



