Awake brain surgery
Overview
Awake brain surgery, also called awake craniotomy, is a type of procedure performed on the brain while you are awake and alert. Awake brain surgery is used to treat some brain (neurological) conditions, including some brain tumors or epileptic seizures.
If your tumor or the area of your brain where your seizures occur (epileptic focus) is near the parts of your brain that control vision, movement or speech, you may need to be awake during surgery. Your surgeon may ask you questions and monitor the activity in your brain as you respond.
Your responses help your surgeon to ensure that he or she treats the correct area of your brain needing surgery. The procedure also lowers the risk of damage to functional areas of your brain that could affect your vision, movement or speech.
Why it's done
If a tumor or section of your brain that causes seizures needs surgical removal, doctors must be sure that they are not damaging an area of the brain that affects your language, speech and motor skills.
It's difficult to pinpoint those areas exactly before surgery. Awake brain surgery allows the surgeon to know exactly which areas of your brain control those functions and avoid them.
Risks
Some of the risks of awake brain surgery include:
- Changes in your vision
- Seizures
- Difficulty with speech or learning
- Loss of memory
- Impaired coordination and balance
- Stroke
- Swelling of the brain or too much fluid in the brain
- Meningitis
- Leaking spinal fluid
- Weak muscles
What you can expect
Before surgery
Doctors first will determine if awake brain surgery is the right choice for you. Doctors will also explain what you can expect during the procedure and the benefits and risks of awake brain surgery.
Awake brain surgery offers many advantages. People who have brain tumors or seizure centers (epileptic foci) near functional brain tissue, whose conditions were once thought inoperable, may consider awake brain surgery to reduce complications and the risk of damage to functional brain tissue.
Awake brain surgery may help safely reduce the size of growing brain tumors, which may prolong life and improve quality of life.
As with any brain surgery, awake brain surgery has the potential for risks and complications. These include bleeding, brain swelling, infection, brain damage or death.
Other surgical complications may include seizures, muscle weakness, and problems with memory and thinking.
Before surgery, your neurosurgeon or a speech-language pathologist may ask you to identify pictures and words on cards or on a computer so that your answers can be compared during surgery.
During surgery
An anesthesia specialist (anesthesiologist) will give you some medication to make you sleepy for parts of your awake brain surgery. Your neurosurgeon will apply numbing medications to your scalp to ensure your comfort.
During the procedure, doctors place your head in a fixed position to keep your head still and ensure surgical accuracy. Some of your hair will be clipped. Your surgeon then removes part of your skull to reach your brain.
You'll be sedated and sleepy while part of your skull is removed in the beginning of the surgery, and also when doctors reattach the skull at the end of the surgery. During the surgery, your anesthesiologist will stop administering the sedative medications and allow you to wake up.
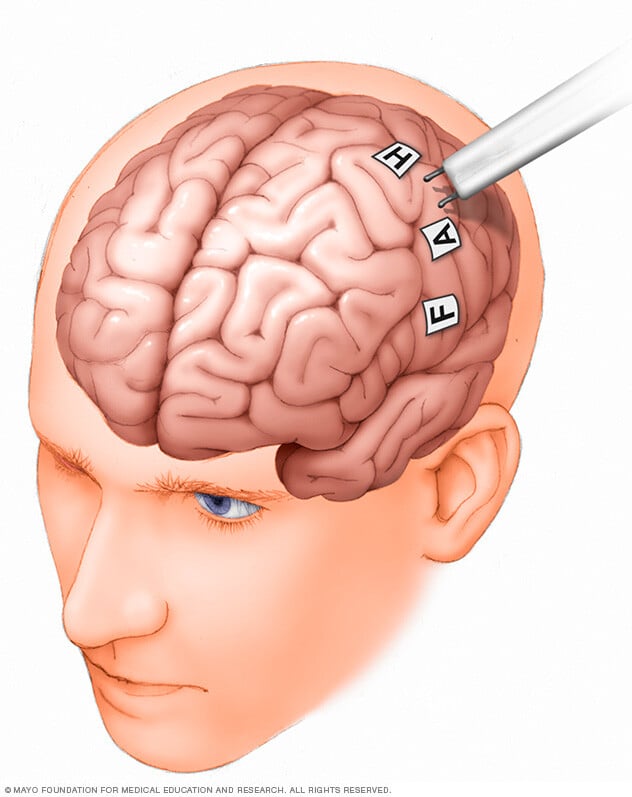
If your brain tumor or epileptic focus is close to areas of your brain that control vision, speech or movement, your doctor will conduct brain mapping. This provides your neurosurgeon with a map of the brain centers that control each of these functions. Your surgeon also can perform brain mapping deeper in your brain during surgery.
Your neurosurgeon uses this map to avoid damaging these areas and preserve these functions. Brain mapping, along with 3-D computer images, allows your surgeon to safely remove as much of your brain tumor or epileptic focus as possible and lower the risks of damaging important body functions.
During surgery, your neurosurgeon or a speech-language pathologist may ask you questions or ask you to identify pictures and words on cards or computer that you saw before surgery. Your doctor may ask you to make movements, identify pictures on cards, count numbers or raise a finger. Your responses help your surgeon identify and avoid the functional areas in your brain.
Your medical team also uses detailed 3-D computer images of your brain taken before and during your surgery, including intraoperative MRI and computer-assisted brain surgery, to guide removal of as much of the brain tumor or epilepsy focus as possible.
Your anesthesiologist and surgical team carefully monitor and assess your body and brain functions and alerts your surgeon if surgery affects brain function.
After surgery
After surgery, your surgeon may request an MRI to ensure that removal of the tumor or epileptic focus is complete.
You'll probably be in the intensive care unit for a while after surgery and spend about two to three days in the hospital.
You generally may return to work and normal activities in six weeks to three months. You'll have a follow-up appointment with your doctor about three months after surgery.
Results
If you had awake brain surgery to manage epilepsy, you generally should see improvements in your seizures after surgery. Some people are seizure-free, while others experience fewer seizures than before the surgery. Occasionally, some people have no change in the frequency of their seizures.
If you had awake brain surgery to remove a tumor, your neurosurgeon generally should have been able to remove most of the tumor. You may still need other treatments, such as radiation therapy or chemotherapy, to help destroy remaining parts of the tumor.



