Prostate biopsy
Overview

A prostate biopsy is a procedure to remove samples of suspicious tissue from the prostate. The prostate is a small, walnut-shaped gland in males that produces fluid that nourishes and transports sperm.
During a prostate biopsy a needle is used to collect a number of tissue samples from your prostate gland. The procedure is performed by a doctor who specializes in the urinary system and male sex organs (urologist).
Your urologist may recommend a prostate biopsy if results from initial tests, such as a prostate-specific antigen (PSA) blood test or digital rectal exam, suggest that you may have prostate cancer. Tissue samples from the prostate biopsy are examined under a microscope for cell abnormalities that are a sign of prostate cancer. If cancer is present, it is evaluated to determine how quickly it's likely to progress and to determine your best treatment options.
Why it's done
A prostate biopsy is used to detect prostate cancer.
Your doctor may recommend a prostate biopsy if:
- A PSA test shows levels higher than normal for your age
- Your doctor finds lumps or other abnormalities during a digital rectal exam
- You've had a previous biopsy with a normal result, but you still have elevated PSA levels
- A previous biopsy revealed prostate tissue cells that were abnormal but not cancerous
Risks
Risks associated with a prostate biopsy include:
- Bleeding at the biopsy site. Rectal bleeding is common after a prostate biopsy.
- Blood in your semen. It's common to notice red or rust coloring in your semen after a prostate biopsy. This indicates the presence of blood, and it's not a cause for concern. Blood in your semen may persist for a few weeks after the biopsy.
- Blood in your urine. This bleeding is usually minor.
- Difficulty urinating. Prostate biopsy can sometimes cause difficulty with urination after the procedure. Rarely, a temporary urinary catheter must be inserted.
- Infection. Rarely, a prostate biopsy can cause an infection of the urinary tract or prostate that requires treatment with antibiotics.
How you prepare
To prepare for your prostate biopsy, your urologist may have you:
- Provide a urine sample to analyze for a urinary tract infection. If you have a urinary tract infection, your prostate biopsy will likely be postponed while you take antibiotics to clear the infection.
- Stop taking medication that can increase the risk of bleeding — such as warfarin (Jantoven), aspirin, ibuprofen (Advil, Motrin IB, others) and certain herbal supplements — for several days before the procedure.
- Do a cleansing enema at home before your biopsy appointment.
- Take antibiotics before your prostate biopsy to help prevent infection from the procedure.
What you can expect
Types of prostate biopsy procedures
Prostate biopsy samples can be collected in different ways. Your prostate biopsy may involve:
- Passing the needle through the wall of the rectum (transrectal biopsy). This is the most common way of performing a prostate biopsy.
- Inserting the needle through the area of skin between the anus and scrotum (transperineal biopsy). A small cut is made in the area of skin (perineum) between the anus and the scrotum. The biopsy needle is inserted through the cut and into the prostate to draw out samples of tissue. An MRI or CT scan is generally used to guide this procedure.
What to expect during transrectal prostate biopsy
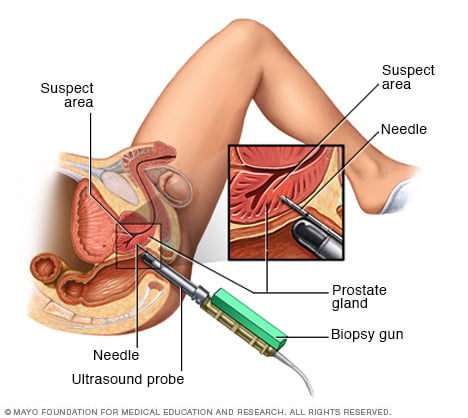
You will be asked to lie on your side with your knees pulled up to your chest. You might be asked to lie on your stomach. After cleaning the area and applying gel, your doctor will gently insert a thin ultrasound probe into your rectum.
Transrectal ultrasonography uses sound waves to create images of your prostate. Your doctor will use the images to identify the area that needs to be numbed with an injection to reduce discomfort associated with the biopsy. The ultrasound images are also used to guide the prostate biopsy needle into place.
Once the area is numbed and the biopsy device is situated, your doctor will retrieve thin, cylindrical sections of tissue with a spring-propelled needle. The procedure typically causes a very brief uncomfortable sensation each time the spring-loaded needle takes a sample.
Your doctor may target a suspicious area to biopsy or may take samples from several places in your prostate. Generally, 10 to 12 tissue samples are taken. The entire procedure usually takes about 20 minutes.
After the procedure
Your doctor will likely recommend that you do only light activities for 24 to 48 hours after your prostate biopsy.
Your doctor might recommend taking an antibiotic for a few days. You might also:
- Feel slight soreness and have some light bleeding from your rectum.
- Have blood in your urine or stools for a few days.
- Notice that your semen has a red or rust-colored tint caused by a small amount of blood in your semen. This can last for several weeks.
Call your doctor if you have:
- Fever
- Difficulty urinating
- Prolonged or heavy bleeding
- Pain that gets worse
Results
A doctor who specializes in diagnosing cancer and other tissue abnormalities (pathologist) will evaluate the prostate biopsy samples. The pathologist can tell if the tissue removed is cancerous and, if cancer is present, estimate how aggressive it is. Your doctor will explain the pathologist's findings to you.
Your pathology report may include:
- A description of the biopsy sample. Sometimes called the gross description, this section of the report might evaluate the color and consistency of the prostate tissue.
- A description of the cells. Your pathology report will describe the way the cells appear under the microscope. Prostate cancer cells may be referred to as adenocarcinoma. Sometimes the pathologist finds cells that appear abnormal but aren't cancerous. Words used to describe these noncancerous conditions include "prostatic intraepithelial neoplasia" and "atypical small acinar proliferation."
- Cancer grading. If the pathologist finds cancer, it's graded on a scale called the Gleason score. Gleason scoring combines two numbers and can range from 2 (nonaggressive cancer) to 10 (very aggressive cancer), though the lower part of the range isn't used as often. Most Gleason scores used to assess prostate biopsy samples range from 6 to 10. A score of 6 indicates a low-grade prostate cancer. A score of 7 indicates a medium-grade prostate cancer. Scores from 8 to 10 indicate high-grade cancers.
- The pathologist's diagnosis. This section of the pathology report lists the pathologist's diagnosis. It may also include comments, such as whether other tests are recommended.



