Premature ventricular contractions (PVCs)
Overview
Premature ventricular contractions (PVCs) are extra heartbeats that begin in one of the heart's two lower pumping chambers (ventricles). These extra beats disrupt the regular heart rhythm, sometimes causing a sensation of a fluttering or a skipped beat in the chest.
Premature ventricular contractions are a common type of irregular heartbeat (arrhythmia). PVCs are also called:
- Premature ventricular complexes
- Ventricular premature beats
- Ventricular extrasystoles
Occasional premature ventricular contractions in people without heart disease usually aren't a concern and likely don't need treatment. You might need treatment if the premature ventricular contractions are very frequent or bothersome, or if you have an underlying heart condition.
Symptoms
Premature ventricular contractions often cause few or no symptoms. But the extra beats can cause unusual sensations in the chest, such as:
- Fluttering
- Pounding or jumping
- Skipped beats or missed beats
- Increased awareness of the heartbeat
When to see a doctor
If you feel fluttering, pounding or a sensation of skipped heartbeats in your chest, talk to your health care provider. A health care provider can determine if the sensations are due to a heart condition or other health concern. Similar signs and symptoms can be caused by many other conditions such as anxiety, low red blood cell count (anemia), overactive thyroid (hyperthyroidism) and infections.
Causes
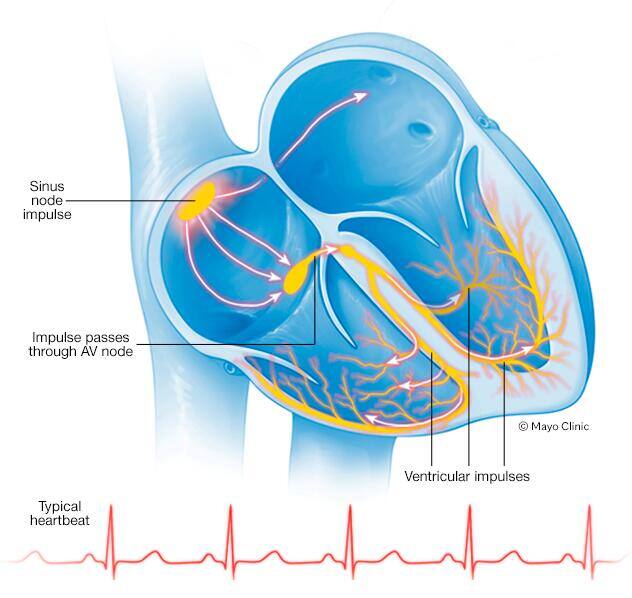
To understand the cause of premature ventricular contractions (PVCs), it might help to learn more about how the heart typically beats.
The heart is made of four chambers — two upper chambers (atria) and two lower chambers (ventricles).
The heart's rhythm is controlled by a natural pacemaker (the sinus node) in the right upper chamber (atrium). The sinus node sends electrical signals that typically start each heartbeat. These electrical signals move across the atria, causing the heart muscles to squeeze (contract) and pump blood into the ventricles.
Next, the signals arrive at a cluster of cells called the AV node, where they slow down. This slight delay allows the ventricles to fill with blood. When the electrical signals reach the ventricles, the chambers contract and pump blood to the lungs or to the rest of the body.
In a typical heart, this heart signaling process usually goes smoothly, resulting in a resting heart rate of 60 to 100 beats a minute.
PVCs are irregular contractions that start in the ventricles instead of the atria. The contractions usually beat sooner than the next expected heartbeat.
The cause of premature ventricular contractions isn't always clear. Certain things including heart diseases or changes in the body can make cells in the lower heart chambers electrically unstable. Heart disease or scarring may cause the heart's signals to be misrouted.
Premature ventricular contractions may be caused by:
- Certain medications, including decongestants and antihistamines
- Alcohol or drug misuse
- Stimulants such as caffeine or tobacco
- Increased levels of adrenaline in the body due to exercise or anxiety
- Injury to the heart muscle due to disease
Risk factors
Certain lifestyle choices and health conditions may make a person more likely to develop premature ventricular contractions (PVCs).
Risk factors for PVCs include:
- Caffeine
- Tobacco
- Alcohol
- Stimulants such as cocaine or methamphetamines
- Exercise — if you have certain types of PVCs
- Anxiety
- Heart attack
- Heart disease, including congenital heart disease, coronary artery disease, heart failure and a weakened heart muscle (cardiomyopathy)
Complications
Having frequent premature ventricular contractions (PVCs) or certain patterns of them might increase the risk of developing irregular heart rhythms (arrhythmias) or weakening of the heart muscle (cardiomyopathy).
Rarely, when accompanied by heart disease, frequent premature contractions can lead to chaotic, dangerous heart rhythms and possibly sudden cardiac death.
Diagnosis
To diagnose premature ventricular contractions (PVCs), a health care provider will typically listen to your heart with a stethoscope. You may be asked questions about your lifestyle habits and medical history.
Tests are done to confirm a diagnosis of premature ventricular contractions.
Tests
An electrocardiogram (ECG or EKG) can detect the extra beats and identify the pattern and source.
An ECG is a quick and painless test to record the heart's electrical activity. Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which displays the test results. An ECG can show if the heart is beating too fast, too slow or not at all.
If you don't have PVCs very often, a standard ECG may not detect them. Your health care provider may ask you to use a portable ECG device at home to obtain more information about your heartbeats. Portable ECG devices include:
- Holter monitor. This portable ECG device can be worn for a day or more to record the heart's activity during daily activities. Some personal devices, such as smartwatches, offer portable ECG monitoring. Ask your health care provider if this is an option for you.
- Event monitor. This portable ECG device is intended to be worn for up to 30 days or until you have an irregular heart rhythm (arrhythmia) or symptoms. You usually press a button when symptoms occur. But some monitors automatically sense the irregular heartbeats and then start recording.
Your health care provider may also recommend an exercise stress test. This test often involves walking on a treadmill or riding a stationary bike while an ECG is done. An exercise stress test can help determine whether exercise triggers your PVCs.
Treatment
Most people with premature ventricular contractions (PVCs) who don't have heart disease won't need treatment. If you have heart disease, PVCs can lead to more-serious heart rhythm problems (arrhythmias). Treatment depends on the underlying cause.
A health care provider may recommend the following treatment for frequent PVCs:
- Lifestyle changes. Eliminating common PVC triggers — such as caffeine or tobacco — may reduce the number of extra beats and lessen symptoms.
- Medications. Blood pressure medications may be prescribed to reduce the premature contractions. Those used for PVCs may include beta blockers and calcium channel blockers. Drugs to control the heart rhythm also may be prescribed if you have a type of irregular heartbeat called ventricular tachycardia or frequent PVCs that interfere with heart function.
- Radiofrequency catheter ablation. If lifestyle changes and medications don't help reduce the PVCs, a catheter procedure may be done to stop the extra beats. In this procedure, a health care provider threads one or more thin, flexible tubes (catheters) through an artery, usually in the groin, and guides them to the heart. Sensors (electrodes) on the tip of the catheter use heat (radiofrequency) energy to create tiny scars in the heart to block irregular electrical signals and restore the heart rhythm.
Self care
The following self-care strategies can help control premature ventricular contractions (PVCs) and improve heart health:
- Track your triggers. If you have frequent PVCs, keeping a diary of the day and timing of symptoms may be helpful. A diary may help identify foods, drinks or activities that trigger the premature ventricular contractions.
- Modify your substance use. Caffeine, alcohol, tobacco and stimulant drugs are known triggers of premature ventricular contractions. Reducing or avoiding such items may reduce PVC symptoms.
- Manage stress. Anxiety can trigger irregular heartbeats. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to tame stress. If you need help managing anxiety, talk to your health care provider about strategies and medications that may help.
Preparing for your appointment
You're likely to start by seeing your family care provider. You may be referred to a doctor trained in heart diseases (cardiologist).
Here's some information to help you get ready for your appointment.
What you can do
Make a list of:
- Your symptoms, how they feel and when they began
- Key medical information, including other recent health conditions and family history of heart disease
- All medications, vitamins and other supplements you take and their dosages
- Questions to ask your health care provider
Take a friend or relative with you, if possible, to help you remember the information you receive.
For premature ventricular contractions, questions to ask your health care provider include:
- What is likely causing my symptoms?
- What tests do I need?
- What treatment approach do you recommend, if any?
- What lifestyle changes can I make to reduce my symptoms?
- Do I need to eliminate alcohol and caffeine?
- Am I at risk of long-term complications?
- How will you monitor my health over time?
- Do I need to adjust the medications I'm taking for other health conditions?
Don't hesitate to ask other questions.
What to expect from your doctor
Your health care provider is likely to ask you questions, including:
- Do your symptoms come and go? If so, when are they likely to occur?
- Do you drink alcohol? If so, how much?
- Do you use caffeine? If so, how much?
- Do you smoke or use other nicotine products?
- Do you use illegal drugs?
- How often do you feel stressed or anxious? What do you do to manage these feelings?



