Placenta accreta
Overview
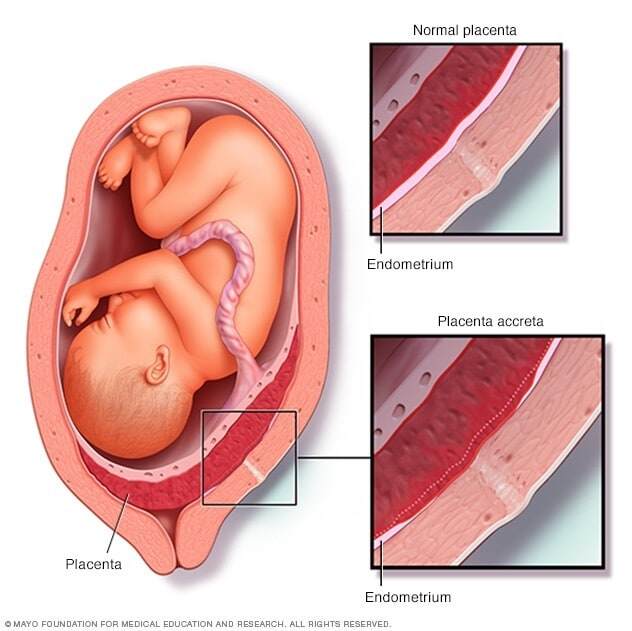
Placenta accreta is a serious pregnancy condition that occurs when the placenta grows too deeply into the uterine wall.
Typically, the placenta detaches from the uterine wall after childbirth. With placenta accreta, part or all of the placenta remains attached. This can cause severe blood loss after delivery.
It's also possible for the placenta to invade the muscles of the uterus (placenta increta) or grow through the uterine wall (placenta percreta).
Placenta accreta is considered a high-risk pregnancy complication. If the condition is diagnosed during pregnancy, you'll likely need an early C-section delivery followed by the surgical removal of your uterus (hysterectomy).
Symptoms
Placenta accreta often causes no signs or symptoms during pregnancy — although vaginal bleeding during the third trimester might occur.
Occasionally, placenta accreta is detected during a routine ultrasound.
Causes
Placenta accreta is thought to be related to abnormalities in the lining of the uterus, typically due to scarring after a C-section or other uterine surgery. Sometimes, however, placenta accreta occurs without a history of uterine surgery.
Risk factors
Many factors can increase the risk of placenta accreta, including:
- Previous uterine surgery. The risk of placenta accreta increases with the number of C-sections or other uterine surgeries you've had.
- Placenta position. If the placenta partially or totally covers your cervix (placenta previa) or sits in the lower portion of your uterus, you're at increased risk of placenta accreta.
- Maternal age. Placenta accreta is more common in women older than 35.
- Previous childbirth. The risk of placenta accreta increases as your number of pregnancies increases.
Complications
Placenta accreta can cause:
- Heavy vaginal bleeding. Placenta accreta poses a major risk of severe vaginal bleeding (hemorrhage) after delivery. The bleeding can cause a life-threatening condition that prevents your blood from clotting normally (disseminated intravascular coagulopathy), as well as lung failure (adult respiratory distress syndrome) and kidney failure. A blood transfusion will likely be necessary.
- Premature birth. Placenta accreta might cause labor to begin early. If placenta accreta causes bleeding during your pregnancy, you might need to deliver your baby early.
Diagnosis
If you have risk factors for placenta accreta during pregnancy — such as the placenta partially or totally covering the cervix (placenta previa) or a previous uterine surgery — your health care provider will carefully examine the implantation of your baby's placenta.
Through an ultrasound or MRI, your health care provider can evaluate how deeply the placenta is implanted in your uterine wall.
Treatment
If your health care provider suspects placenta accreta, he or she will work with you to develop a plan to safely deliver your baby.
In the case of extensive placenta accreta, a C-section followed by the surgical removal of the uterus (hysterectomy) might be necessary. This procedure, also called a cesarean hysterectomy, helps prevent the potentially life-threatening blood loss that can occur if there's an attempt to separate the placenta.
If you have vaginal bleeding during the third trimester, your health care provider might recommend pelvic rest or hospitalization.
Before surgery
Your health care team will include your obstetrician and gynecologist, subspecialists in pelvic surgery, an anesthesia team, and a pediatric team.
Your health care provider will discuss the risks and potential complications associated with placenta accreta. He or she might also also discuss the possibility of your:
- Having a blood transfusion during or after delivery
- Needing to be admitted to the intensive care unit after delivery if you have life-threatening bleeding
During surgery
During your C-section, your health care provider will deliver your baby through an initial incision in your abdomen and a second incision in your uterus. After the delivery, a member of your health care team will remove your uterus — with the placenta still attached — to prevent severe bleeding.
After a hysterectomy, you no longer can become pregnant. If you had planned additional pregnancies in the future, discuss possible options with your health care provider.
Rarely, the uterus and placenta might be kept intact, allowing the placenta to dissolve over time. However, this approach can have serious complications, including:
- Severe vaginal bleeding
- Infection
- The need for a hysterectomy at a later date
In addition, limited research suggests that women who are able to avoid hysterectomy after having placenta accreta are at risk of complications, including recurrent placenta accreta, with later pregnancies.
Coping and support
If your health care provider suspects that you have placenta accreta, you'll likely worry about how your condition will affect your delivery, your baby and, possibly, future pregnancies.
To ease your anxiety:
- Find out about placenta accreta. Gathering information about your condition might help you feel less anxious. Talk to your health care provider, do some research and connect with women who've had placenta accreta.
- Prepare for a C-section. Ask questions about the procedure, pain management and expectations for recovery.
- Prepare for a hysterectomy. After the hysterectomy, you'll no longer have menstrual cycles or be able to get pregnant. Ask your health care provider about what to expect during your recovery, the length of recovery and how the surgery might affect your recovery after giving birth.
- Take care of yourself. Set aside time for soothing activities that help you relax, such as reading or listening to music. Relaxation techniques, including meditation, deep breathing or guided imagery, may help ease stress and produce a feeling of calm.
Preparing for your appointment
If you have vaginal bleeding during your third trimester, contact your health care provider right away. If the bleeding is severe, seek emergency care.
Often, placenta accreta is suspected after an ultrasound early in pregnancy. You can learn about the condition and develop a plan to manage it at a follow-up visit.
What you can do
Before your appointment, you might want to:
- Ask about pre-appointment precautions, such as activities you should avoid and symptoms that should prompt you to seek urgent care.
- Ask a family member or friend to join you to help you remember the information you're given.
- Write down questions to ask your health care provider.
Some questions to ask your health care provider about placenta accreta include:
- What's causing the bleeding?
- What treatment approach do you recommend?
- What care will I need during my pregnancy?
- What signs or symptoms should cause me to call you?
- What signs or symptoms should cause me to go to the hospital?
- Will I be able to deliver vaginally?
- Does this condition increase the risk of complications during future pregnancies?
- Will I need a hysterectomy after the baby is delivered?
Don't hesitate to ask other questions as they occur to you during your appointment.
What to expect from your doctor
Your health care provider is likely to ask you questions, such as:
- When did you notice vaginal bleeding?
- Did you bleed only once, or has the bleeding been off and on?
- How heavy is the bleeding?
- Is the bleeding accompanied by pain or contractions?
- Have you had previous pregnancies?
- Have you had uterine surgeries?
- How long would it take to get to the hospital in an emergency, including time to arrange child care and transportation?