Occupational asthma
Overview
Occupational asthma is a type of asthma caused by breathing in fumes, gases, dust or other substances while on the job. These substances can trigger an immune system response that changes how the lungs work. Occupational asthma also is called work-related asthma.
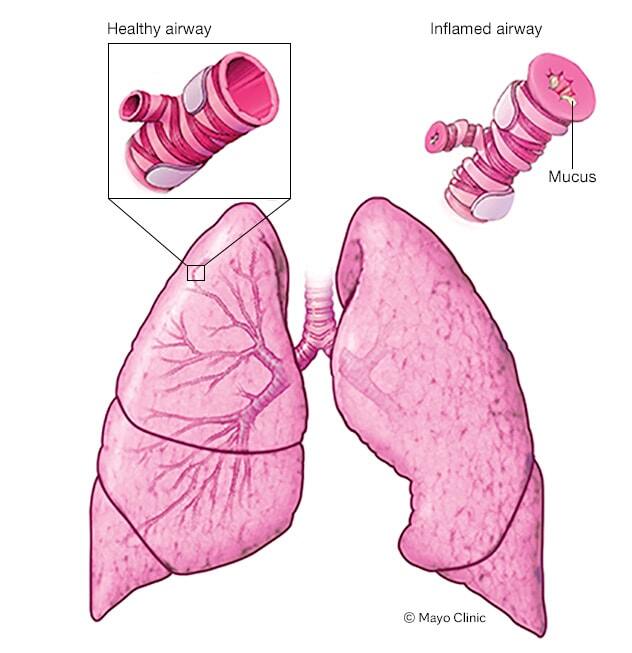
In asthma, the airways narrow and swell. They also may make extra mucus. This makes it difficult to breathe and may cause chest tightness, wheezing and shortness of breath.
Avoiding triggers is important for managing occupational asthma. Treatment includes medicines that reduce symptoms. For people who were diagnosed with asthma in the past, medicines may help improve symptoms related to workplace triggers.
If occupational asthma is not treated and triggers are not avoided, the asthma can cause permanent changes to the lungs.
Symptoms
Occupational asthma symptoms may include:
- Wheezing.
- Coughing.
- Shortness of breath.
- Chest tightness.
Other possible symptoms may include:
- Runny nose.
- Stuffy nose.
- Itchy or watery eyes.
Occupational asthma symptoms depend on the substance you're exposed to, how long and how often you're exposed, and other factors. Your symptoms may:
- Begin right after exposure to a substance, later in the day or after work.
- Improve or go away on days off or during vacations and then return when you go to work.
- May begin early in the day and fail to improve on days off as disease progresses.
- May become permanent even after long periods away from work.
When to see a doctor
Seek medical treatment right away if your symptoms worsen. Severe asthma attacks can be life-threatening. Symptoms of an asthma attack that need emergency treatment include:
- Shortness of breath or wheezing that quickly gets worse.
- No easing of symptoms after using a quick-relief medicine.
- Shortness of breath even with little activity.
Make an appointment to see your healthcare professional if you have breathing problems, such as coughing, wheezing or shortness of breath, especially if the symptoms don't go away or worsen.
Causes
More than 400 workplace substances have been identified as possible triggers of occupational asthma. These substances include:
- Animal proteins found in dander, hair, scales, fur, saliva and body wastes.
- Chemicals used to make paints, varnishes, adhesives, laminates and soldering resin. Other examples include chemicals used to make insulation, packaging materials, and foam mattresses and upholstery.
- Enzymes used in detergents and baking flour.
- Metals, particularly platinum, chromium and nickel sulfate.
- Plant substances, including proteins found in natural rubber latex, flour, cereals, cotton, flax, hemp, rye, wheat and papaya.
- Irritating gases or particles, such as chlorine gas, sulfur dioxide and smoke.
Asthma symptoms start when your lungs become irritated. This irritation causes an immune system reaction called inflammation. Inflammation is defined as swelling and other changes in airway tissues caused by immune system activity. These changes narrow the airways and make it difficult to breathe.
With occupational asthma, lung inflammation may be triggered by a substance that a person is allergic to, such as mold or an animal protein. Sometimes lung inflammation is triggered by an irritating substance, also called an irritant, such as chlorine or smoke.
Risk factors
The more you're exposed to an irritant, the greater the risk of developing occupational asthma. In addition, you will have increased risk if:
- You have existing allergies or asthma. Although this can increase your risk, many people who have allergies or asthma do jobs that expose them to lung irritants and never have symptoms.
- Other family members have allergies or asthma. Your parents may pass down genes that make it more likely for you to develop asthma.
- You work around known asthma triggers. Some substances are known to be lung irritants and asthma triggers.
- You smoke. Smoking increases your risk of developing asthma if you are exposed to certain types of irritants.
High-risk jobs
It's possible to develop occupational asthma in almost any workplace. But your risk is higher in certain workplaces. Some of the riskiest jobs linked to asthma-producing substances include the following:
| Jobs | Asthma-producing substances |
|---|---|
| Adhesive handlers | Chemicals |
| Animal handlers, veterinarians | Animal proteins |
| Bakers, millers, farmers | Cereal grains |
| Carpet-makers | Vegetable gums |
| Metalworkers | Cobalt, nickel |
| Food production workers | Milk powder, egg powder |
| Forest workers, carpenters, cabinetmakers | Wood dust |
| Hairdressers | Dyes |
| Healthcare workers | Latex and chemicals |
| Pharmaceutical workers, bakers | Drugs, enzymes |
| Seafood processors | Herring, snow crab |
| Spray painters, insulation installers, plastics and foam industry workers, welders, metalworkers, chemical manufacturers, shellac handlers | Chemicals |
| Textile workers | Dyes, plastics |
| Users of plastics or epoxy resins, chemical manufacturers | Chemicals |
Complications
The longer you're exposed to a substance that can cause occupational asthma, the worse your symptoms may become. Also, the longer you're exposed, the longer it will take for symptoms to improve after exposure stops. In some cases, exposure to airborne asthma triggers can cause permanent changes to your lungs.
Prevention
The best way to prevent occupational asthma is to control exposure to chemicals and other substances that are known to be irritating. Workplaces can set up controls to prevent exposures, use less harmful substances and provide personal protective equipment (PPE) for workers.
Medicines may help relieve symptoms and control inflammation linked to occupational asthma. But you can do several things on your own to be healthy and lessen the possibility of attacks:
- If you smoke, quit. Being smoke-free may help prevent or lessen symptoms of occupational asthma.
- Get a flu vaccination. This can help prevent illness that affects the lungs.
- Avoid nonsteroidal anti-inflammatory drugs (NSAIDs) and other medicines that may make symptoms worse. Ask your healthcare professional about medicines you take regularly.
- Lose weight. For people with obesity, losing weight can help improve symptoms and overall lung health.
If you are in the United States and you have a high-risk job, your company must follow rules to help protect you from harmful chemicals. Under guidelines from the Occupational Safety and Health Administration (OSHA), your employer is required to do the following:
- Tell you if you'll be working with any harmful chemicals.
- Train you how to safely handle these chemicals.
- Train you how to respond to an emergency, such as a chemical spill.
- Supply protective gear, such as masks and respirators.
- Offer extra training when a new chemical is used at your workplace.
Under OSHA guidelines, your employer is required to keep a material safety data sheet (MSDS) for each harmful chemical used in your workplace. This is a document that must be submitted by the chemical's manufacturer to your employer. You have a legal right to see and copy such documents. If you suspect you're allergic to a certain substance, show the MSDS to your healthcare professional.
While at work, watch for conditions that may not be safe or healthy. Report concerns to your supervisor. If necessary, call OSHA at 800-321-OSHA (
Diagnosis

Diagnosing occupational asthma is similar to diagnosing other types of asthma. However, your healthcare professional also will try to identify whether a workplace substance is causing your symptoms and what substance is causing problems.
An asthma diagnosis needs to be confirmed with a test called a lung function test. This test shows how well your lungs work. An allergy skin prick test can show if you have allergic reactions to some allergy-causing substances. Blood tests, X-rays or other tests may be necessary to rule out a cause other than occupational asthma.
Testing your lung function
Lung function tests include:
-
Spirometry. During this 10- to 15-minute test, you take deep breaths and forcefully exhale into a hose connected to a machine called a spirometer. A spirometer measures how much air your lungs can hold and how quickly you can breathe out. This is the preferred test for diagnosing asthma.
You will repeat the test after inhaling asthma medicine that helps open airways. Improved lung function after using the medicine supports a diagnosis of asthma.
-
Peak flow measurement. You may be asked to carry a small hand-held device called a peak flow meter. This device measures how quickly you can force air out of your lungs. The slower you exhale, the worse your condition.
You'll likely be asked to use your peak flow meter at certain times during working and nonworking hours. If your breathing improves significantly when you're away from work, you may have occupational asthma.
Tests for causes of occupational asthma
You may need tests to see whether you have a reaction to specific substances. These include:
- Allergy skin tests. During a skin test, small amounts of common allergy-causing substances are scratched into your skin. Then the area is observed for about 15 minutes. Swelling or a change in skin color indicates an allergy to the substance. These tests can show an allergy to animals, mold, dust mites, plants and latex. They can't be used to measure a reaction to chemicals.
- Challenge test. You inhale a mist containing a small amount of a suspected chemical to see if it triggers a reaction. Your lung function will be tested before and after the test is given to see if the chemical affects your ability to breathe.
- Chest X-ray. Occupational asthma is one kind of occupational lung disease. You might need a chest X-ray to diagnose other kinds of job-related breathing problems.
Treatment
The goal of treatment is to prevent symptoms and stop an asthma attack in progress.
Avoiding the workplace substance that causes your symptoms is important. Once you become sensitive to a substance, tiny amounts may trigger asthma symptoms, even if you wear a mask or respirator.
You may need medicines for successful treatment. The same medicines are used to treat both occupational and nonoccupational asthma.
The right medicine for you depends on many things. These include your age, symptoms, asthma triggers and what seems to work best to keep your asthma under control.
Long-term control medicines
- Inhaled corticosteroids. Inhaled corticosteroids reduce inflammation and have a relatively low risk of side effects.
- Leukotriene modifiers. These medicines are alternatives to corticosteroids. Sometimes, they're taken with corticosteroids.
- Long-acting beta agonists (LABAs). LABAs open the airways and reduce inflammation. For asthma, LABAs generally should only be taken in combination with an inhaled corticosteroid.
- Combination inhalers. These medicines contain a LABA and a corticosteroid.
Quick-relief, short-term medications
- Short-acting beta agonists. These medicines ease symptoms during an asthma attack.
- Oral and intravenous corticosteroids. These relieve airway inflammation for severe asthma. These are taken by mouth or given as a shot. Over the long term, they cause serious side effects.
If you need to use a quick-relief inhaler more often than recommended, you may need to adjust your long-term control medicine.
Also, if allergies trigger or worsen your asthma, you may benefit from allergy treatments. These treatments include medicines taken by mouth or with a nasal spray. Antihistamines help block some immune system activity that causes allergy symptoms. Decongestants help relieve a stuffy nose.
Alternative medicine
Many people claim alternative remedies reduce asthma symptoms. But in most cases, more research is needed to see if they work and if they have possible side effects. Alternative remedies that need further study include:
- Breathing techniques. These include structured breathing programs such as the Buteyko method, the Papworth method, lung-muscle training and yoga breathing exercises. While these techniques may help improve quality of life, they have not proved to improve asthma symptoms.
- Acupuncture. This technique has roots in traditional Chinese medicine. It involves placing very thin needles at strategic points on the body. Acupuncture is safe and generally painless, but there is not enough evidence to show it treats asthma.
Preparing for an appointment
You're likely to start by seeing your primary healthcare professional. Or you may start by seeing a doctor who specializes in asthma, such as an allergist-immunologist or a pulmonologist.
Here's some information to help you prepare for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance. You may need to stop taking antihistamines if you're likely to have an allergy skin test.
- Write down any symptoms you're experiencing, including any that do not seem related to problems with breathing.
- Note the timing of your asthma symptoms — for example, note if your symptoms are worse at work and get better when you're away from work.
- Make a list of all possible workplace lung irritants and anything else that seems to trigger your symptoms. You may want to take a look at the material safety data sheet (MSDS) for your work area, if there is one. This sheet lists toxic substances and irritants used on your job site. Keep in mind, not all occupational asthma triggers are listed in the MSDS.
- Write down key personal information, including major stresses or recent life changes and changes in your job or workplace.
- Bring a list of all medicines, vitamins or supplements you take.
- Bring a family member or friend along, if possible. Someone who accompanies you may remember information you missed or forgot.
- Write down questions to ask your care healthcare professional.
For occupational asthma, some basic questions to ask include:
- Is a workplace irritant a likely cause of my breathing problems or asthma attacks?
- What are other possible causes for my symptoms or condition?
- What tests do I need? Do these tests require any special preparation?
- Is my condition likely temporary or chronic?
- How do I treat occupational asthma? Do I have to quit my job?
- What are the alternatives to the treatment you're suggesting?
- I have other health conditions. How can I best manage these conditions together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed material I can take with me? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your healthcare professional is likely to ask you several questions, such as:
- When did you first notice your symptoms?
- If you already use asthma medicine, how often do you use a quick-relief inhaler?
- Do you have breathing problems when you're away from work or only when you're on the job?
- Have your symptoms been continuous, or do they come and go?
- Have you been diagnosed with allergies or asthma?
- Are you exposed to fumes, gases, smoke, irritants, chemicals, or plant or animal substances at work? If so, how often and for how long?
- Do you work in unusual environmental conditions, such as extreme heat, cold or dryness?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do other members of your family have allergies or asthma?



