Functional dyspepsia
Overview
Functional dyspepsia (dis-PEP-see-uh) is a term for recurring symptoms of an upset stomach that have no obvious cause. Functional dyspepsia also is called nonulcer dyspepsia.
Functional dyspepsia is common. It is a constant condition but symptoms don't happen all the time. Symptoms resemble those of an ulcer. They include pain or discomfort in the upper abdomen, bloating, belching and nausea.
Symptoms
Symptoms of functional dyspepsia may include:
- Pain or burning in the stomach, bloating, excessive belching, or nausea after eating
- An early feeling of fullness when eating. The feeling of fullness also is called satiety.
- Stomach pain that occurs unrelated to meals or goes away when eating.
When to see a doctor
Make an appointment with your health care provider if you experience persistent symptoms that worry you.
Seek medical attention right away if you experience:
- Bloody vomit.
- Dark, tarry stools.
- Shortness of breath.
- Pain in your jaw, neck or arm.
- Unexplained weight loss.
Causes
No one knows what causes functional dyspepsia. Health care providers consider it a functional disorder. That means it can't be explained by a medical condition, so routine testing may not show any problems or causes. As a result, the diagnosis is based on symptoms.
Risk factors
Some factors can increase the risk of functional dyspepsia. They include:
- Being female.
- Using certain pain relievers that are available without a prescription. These include aspirin and ibuprofen (Advil, Motrin IB, others), which can cause stomach problems.
- Smoking.
- Anxiety or depression.
- History of childhood physical or sexual abuse.
- Helicobacter pylori infection.
Diagnosis
Your health care provider most likely will review your symptoms and perform a physical exam. Several tests can help find the cause of your discomfort and rule out other disorders. These may include:
- Blood tests. Blood tests may help rule out other diseases that can cause symptoms like those of functional dyspepsia.
- Tests for a bacterium. A bacterium called Helicobacter pylori (H. pylori). H. pylori can cause stomach problems. H. pylori testing may involve a stool sample, the breath, or tissue samples of the stomach taken during endoscopy.
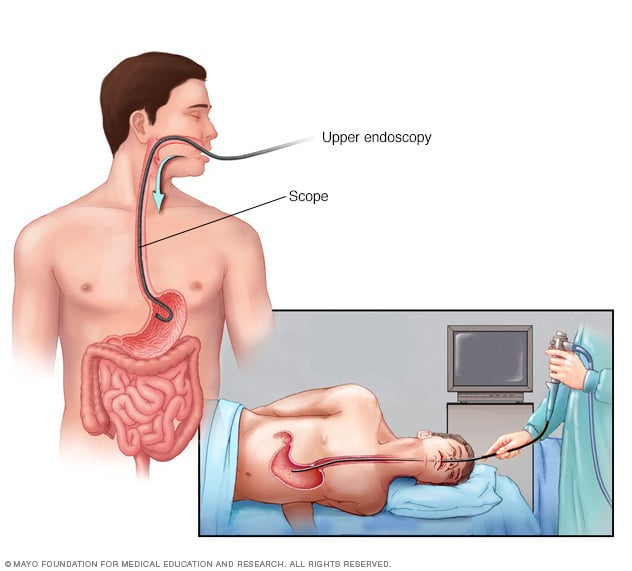
- Endoscopy. A special tube with a camera lens and light is passed down the throat and into the esophagus, stomach and the upper part of the small intestine. This tube is called an endoscope. This allows the doctor to collect tissue samples to look for infection or inflammation.
In some cases, you may have other tests to see how well your stomach empties its contents.
Treatment
Functional dyspepsia that can't be managed with lifestyle changes may need treatment. Treatment depends on your symptoms. It may combine medicines and behavior therapy.
Medicines
Some medicines may help manage symptoms of functional dyspepsia. They include:
- Gas remedies that are available without a prescription. An ingredient called simethicone may provide some relief by reducing intestinal gas. Examples of gas-relieving remedies include Mylanta and Gas-X.
- Medicines to reduce acid production. These medicines are called H-2-receptor blockers and are available without a prescription. They include cimetidine (Tagamet HB), famotidine (Pepcid AC) and nizatidine (Axid AR). Stronger versions of these medicines also are available by prescription.
-
Medicines that block acid "pumps." Medicines called proton pump inhibitors shut down the acid "pumps" within acid-secreting stomach cells.
Proton pump inhibitors available without a prescription include lansoprazole (Prevacid 24HR), omeprazole (Prilosec OTC) and esomeprazole (Nexium 24HR). Proton pump inhibitors also are available by prescription.
- Antibiotics. If tests find H. pylori in your stomach, your health care provider may prescribe antibiotics along with acid-suppressing medicine.
- Low-dose antidepressants. Your provider may prescribe low doses of tricyclic antidepressants and antidepressants known as selective serotonin reuptake inhibitors. These medicines may inhibit the activity of neurons that control intestinal pain.
- Prokinetics. These medicines help your stomach empty faster and tighten the valve between your stomach and esophagus. This helps to reduce upper abdominal pain.
- Medicines to relieve nausea. These medicines are called anti-emetics. If you feel like throwing up after eating, anti-emetics may help. These include promethazine, prochlorperazine and meclizine.
Behavior therapy
Working with a counselor or therapist may relieve symptoms that aren't helped by medicines. A counselor or therapist can show you relaxation techniques to help you cope with your symptoms. You may also learn ways to reduce stress to help manage your symptoms.
Lifestyle and home remedies
Your health care provider may recommend lifestyle changes to help you control your functional dyspepsia.
Make changes to your diet
Changes to what you eat and how you eat might help control your symptoms. Try to:
-
Eat smaller, more-frequent meals. Having an empty stomach sometimes contributes to functional dyspepsia. Nothing but acid in your stomach may make you feel sick. Try eating a small snack such as a cracker or a piece of fruit.
Try not to skip meals. Avoid large meals and overeating. Eat smaller meals more often.
- Stay away from trigger foods. Some foods may trigger functional dyspepsia. These may include fatty and spicy foods, carbonated beverages, caffeine, and alcohol.
- Chew your food slowly and completely. Allow time to enjoy your meals.
Reduce stress in your daily life
Stress-reduction techniques or relaxation therapy may help you manage your symptoms. To reduce stress, spend time doing hobbies, sports and other things you enjoy.
Alternative medicine
People with functional dyspepsia often turn to complementary and alternative medicines to help them cope. Further studies are needed before complementary and alternative medicines can be recommended. But they may provide some symptom relief when used with other approaches suggested by your health care provider.
If you're interested in complementary and alternative treatments, talk to your provider about:
-
Herbal supplements. A combination of peppermint and caraway oils may offer some benefit for functional dyspepsia. Together, they relieved pain symptoms in a l-week trial. Iberogast contains extracts of nine herbs. It may relieve gastrointestinal spasms and improve the intestine's ability to move food.
A Japanese herbal remedy called rikkunshito also may be helpful. Researchers found it improved abdominal pain, heartburn and bloating better than placebo. A placebo is a treatment with no therapeutic effect that looks the same as, and is given the same way as, the medicine or treatment being tested in a study. Artichoke leaf extract may reduce symptoms of functional dyspepsia.
- Relaxation techniques. Relaxing activities may help you cope with your symptoms. Meditation, exercise or other activities may help manage your stress.
Preparing for an appointment
You may start by seeing your primary care provider. Or you may be referred right away to a doctor who specializes in the treatment of diseases of the stomach and intestines (gastroenterologist).
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medications, vitamins or supplements you take, including the doses
- Questions to ask your provider.
Take a family member or friend along, if possible, to help you remember the information you're given.
For functional dyspepsia, some basic questions to ask your provider include:
- What's likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What's the best course of action?
- What are the alternatives to the primary approach you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your provider is likely to ask you several questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
What you can do in the meantime
Avoid doing anything that seems to worsen your symptoms.