Mumps
Overview
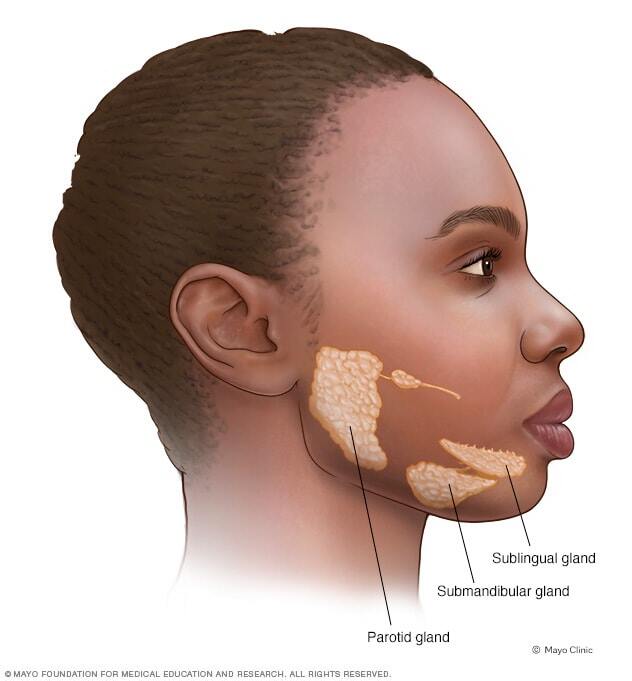
Mumps is an illness caused by a virus. It usually affects the glands on each side of the face. These glands, called parotid glands, make saliva. Swollen glands may be tender or painful.
Mumps are not common in the United States because of vaccines. But outbreaks do happen. People who are not vaccinated are at high risk of infection. Vaccinated people who get mumps usually have milder symptoms and fewer complications.
There is no specific medicine for mumps. Treatment relieves pain and discomfort.
Symptoms

Symptoms of mumps show up about 2 to 3 weeks after exposure to the virus. Some people may have no symptoms or very mild symptoms.
The first symptoms may be similar to flu symptoms such as:
- Fever.
- Headache.
- Muscle aches or pain.
- Not wanting to eat.
- Tiredness.
Swelling of the salivary glands usually starts within a few days. Symptoms may include:
- Swelling of one or both glands on the sides of the face.
- Pain or tenderness around the swelling.
- Less often, swelling of glands below the floor of the mouth.
When to see a doctor
See your health care provider if you or your child has symptoms of mumps. Mumps spreads very easily for about five days after the swelling starts. If you think you have mumps, let the clinic know before you go. The clinic staff likely will take steps to prevent the spread of disease.
Other conditions may have similar symptoms, so it's important to get a quick diagnosis.
If you think your child has mumps, call your care provider if your child develops:
- Fever of 103 F (39 C) or greater.
- Trouble eating or drinking.
- Confusion or disorientation.
- Stomach pain.
- Pain and swelling of the testicles.
In the meantime:
- Rest as much as possible.
- Use pain relievers you can get without a prescription, such as ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
- Use a cold or warm cloth over swollen salivary glands.
Causes
Mumps is caused by a type of germ called a virus. When someone has mumps, the virus is in saliva. Coughing or sneezing can release tiny droplets with the virus into the air.
You can get the virus by breathing in tiny droplets. Or you can get the virus by touching a surface where droplets have landed and then touching your face. You also can pick up the virus from direct contact, such as kissing or sharing a water bottle.
Outbreaks in the United States most often happen where people live or work in close contact. These may include college campuses, summer camps and schools.
Complications
Complications of mumps are more likely among people who aren't vaccinated. They can happen even if a person didn't have swollen salivary glands.
Complications happen when the virus reaches other tissues in the body. Complications may include:
- Swollen testicles. This complication, also called orchitis, causes severe pain. It's more common with a mumps infection after puberty. A swollen testicle may lead to a decrease in the size of the testicle and a decline in fertility.
- Swollen ovaries. This complication, also caused oophoritis, causes pain, upset stomach, vomiting and fever. This complication is more likely after puberty. The condition doesn't seem to affect fertility.
- Encephalitis. Encephalitis is swelling, called inflammation, in the brain that may damage tissues. This complication can cause changes in consciousness, seizures and loss of muscle control.
- Meningitis. Meningitis is swelling, or inflammation, of the membranes around the brain and spinal cord. It may cause head, fever and neck stiffness. Meningitis related to mumps rarely causes long-term problems.
- Hearing loss. This complication can happen suddenly or over time. Hearing usually gets better after the illness.
- Pancreatitis. Mumps can cause damage to the pancreas, called pancreatitis, from swelling. Symptoms may include pain or tenderness near the stomach, upset stomach, vomiting and fever.
- Miscarriage. Getting mumps during the first 12 weeks of pregnancy may increase the risk that a pregnancy will end, called miscarriage.
Prevention
Most people who have had the mumps vaccines, called fully vaccinated, are protected from mumps infections. People who aren't vaccinated are more likely to get mumps.
For some people, vaccine protection may go down over time. When fully vaccinated people get mumps, they usually have milder symptoms and fewer complications.
The MMR vaccine
The mumps vaccine is a part of the recommended childhood vaccinations. It's usually given as a combined measles-mumps-rubella (MMR) vaccine. The schedule is:
- The first dose between the ages of 12 and 15 months.
- The second dose between the ages of 4 and 6 years before entering school.
Another version of MMR includes the vaccine against the virus that causes chickenpox, called varicella-zoster virus. But that vaccine, called the measles-mumps-rubella-varicella vaccine (MMRV) is not used for the first dose in the standard vaccination schedule for children.
Extensive studies in several countries have shown that there is no link between the MMR or MMRV vaccines and autism. The original study that suggested this connection in 1998 was based on scientific errors. That study was removed from the scientific record in 2010.
Extensive reports from the American Academy of Pediatrics, the National Academy of Medicine, and the Centers for Disease Control and Prevention conclude that there is no scientifically proven link between the MMR vaccine and autism.
People who need the MMR vaccine
If you haven't had two doses or aren't sure, talk to your health care provider. You may need two doses of the vaccine or a booster. This is especially important if you are in a high-risk setting or in an outbreak. The following people may need proof of vaccination or more doses:
- College students.
- People in the military.
- International travelers.
- Health care workers.
People who don't need the MMR vaccine
If you're not sure if you're vaccinated, a blood test can show whether you have antibodies to mumps. If you have antibodies to the virus, then your immune system would fight a mumps infection and you don't need another vaccine.
People who were born before 1957 were likely exposed to the virus. They likely are immune to mumps.
The mumps vaccine is made from a weak but still infectious mumps virus. A typical immune system can handle this weak virus easily. But people with immune systems that won't respond quickly or strongly to the vaccine don't usually get this vaccine. But there are some exceptions if the benefits outweigh the risks. Also, this type of vaccine is not suggested for people who are pregnant.
Side effects of the MMR vaccine
The MMR vaccine is safe and effective. Most people have no side effects.
If they happen, mild side effects may include:
- Soreness at the site of the shot.
- Fever.
- Rash at the site of the shot.
- Swelling of the glands in the cheeks or neck.
In rare cases, some people may have symptoms such as pain and stiffness in joints, seizures, short-term drop in blood platelets or a rash.
Severe allergic reactions are rare. People who have a severe allergic reaction to the first dose aren't given a second dose. Also, people won't get the vaccine if they've had a severe allergic reaction to an ingredient in the vaccine.
Diagnosis
A care provider may diagnose mumps based on typical symptoms and known exposure to mumps. Tests used to look for the virus and diagnose mumps include:
- A test of a sample from the mouth.
- A blood test that may show an immune system reaction to the virus.
- A test of a sample of urine, but this is less common.
Treatment
There is no specific treatment for mumps. Most people recover within 3 to 10 days.
Steps you can take to aid recovery and lessen symptoms include:
- Rest.
- Pain relievers that you can get without a prescription such as ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
- A cold or warm cloth for swollen salivary glands.
- A cold cloth or ice pack for swollen testicles.
- Drinking plenty of fluids.
It's important to isolate yourself or your child during the illness to prevent spreading the infection. Avoid contact with others until at least five days after the start of swollen salivary glands.
Preparing for your appointment
What you can do
- Write down symptoms you or your child has had, and for how long.
- Try to remember if you or your child has been exposed to someone with signs and symptoms of mumps within the last few weeks.
- Make a list of all medications, vitamins or supplements that your or your child takes.
- Write down key medical information, including other diagnosed conditions.
- Write down key personal information, including any recent changes or stressors in your life.
- Write down questions to ask your doctor.
Questions to ask your doctor
- What's the most likely cause of these signs and symptoms?
- What treatment approach do you recommend?
- How soon should symptoms improve?
- Are there are home remedies or self-care steps that could help relieve symptoms?
- Am I or is my child contagious? For how long?
- What steps should we take to reduce the risk of infecting others?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask questions during your appointment.
If you think you or your child has mumps, contact your health care provider.
What to expect from your doctor
Be prepared to answer the following questions:
- What symptoms have you had? When did they begin?
- When did you first notice swelling in your face?
- Have you had pain? Where?
- Do you know if you've recently been exposed to mumps?
- Do you know your current vaccination status?
- Has anyone in your home had symptoms?
- What drugs, vitamins, herbal remedies or dietary supplements do you take regularly?



