Moles
Overview

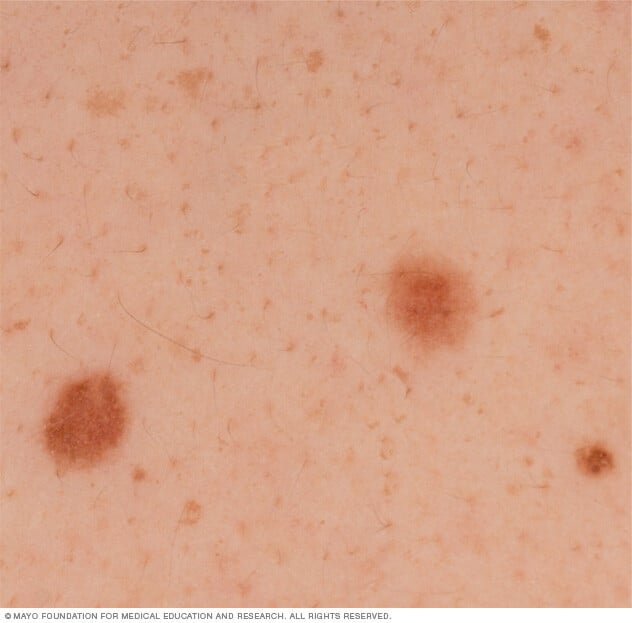
Moles, also known as nevi, are a common type of skin growth. They often appear as small, dark brown spots that are caused by clusters of pigment-forming cells called melanocytes. Most people have 10 to 45 moles that appear during childhood and the teenage years. How these moles look may change over time. They also may fade over time.
Most moles are harmless. Rarely, they become cancerous. Being aware of changes in your moles and other pigmented patches is important to finding skin cancer, especially malignant melanoma.
Symptoms
The typical mole is a small brown spot. But moles come in different colors, shapes and sizes:
- Color and texture. Moles can be brown, tan, black, blue, red or pink. They can be smooth, wrinkled, flat or raised. They may have hair growing from them.
- Shape. Most moles are oval or round.
- Size. Moles are typically less than 1/4 inch (about 6 mm) in diameter — the size of a pencil eraser. Those present at birth, known as congenital nevi, can be bigger and cover part of the face, trunk or a limb.
Moles can grow anywhere on your body, including your scalp and armpits, as well as under your nails and between your fingers and toes. Most people have 10 to 45 moles. Many of these moles occur by age 40. Moles may change or fade away over time. They may become darker and larger with hormonal changes that occur during the teenage years and while pregnant.
Clusters of brown spots around the eyes, cheeks and nose are dermatoses papulosa nigra — a type of seborrheic keratosis that is noncancerous and appears as waxy brown, black or tan growths. They aren't clusters of pigment-forming cells, known as nevi. Dermatoses papulosa nigra are more common among Black women. These lesions don't carry a risk of melanoma, but they can be treated as a cosmetic concern.
Unusual moles that may indicate melanoma
A mole may be a sign of skin cancer if it has irregular borders or an asymmetrical shape, or if it changes in color, shape, size or height. This ABCDE guide can help you remember what to watch for:
- A is for asymmetrical shape. One half is unlike the other half.
- B is for border. Look for moles with irregular, notched or scalloped borders.
- C is for changes in color. Look for growths that have changed color, have many colors or have uneven color.
- D is for diameter. Look for new growth in a mole larger than 1/4 inch (about 6 mm).
- E is for evolving. Watch for moles that change in size, shape, color or height. Also, new symptoms can arise, such as itchiness or bleeding.
Cancerous moles, also known as malignant moles, vary greatly in how they look. Some may show all of the changes listed above. Others may have only one or two unusual traits.
When to see a doctor
Make an appointment with your healthcare professional if a mole looks unusual, grows or otherwise changes.
Causes
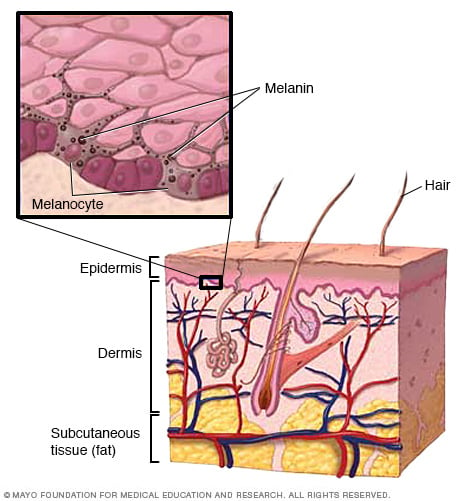
Moles are caused when cells in the skin called melanocytes grow in clusters. Melanocytes generally are distributed throughout the skin. They produce melanin, the natural pigment that gives skin its color.
Complications
Melanoma is the main complication of moles. Some people have an above-average risk of their moles becoming cancerous and leading to melanoma. Factors that raise melanoma risk include:
- Being born with large moles. These type of moles are called congenital nevi. They are subclassified based on their estimated adult size. Large and giant congenital nevi that are more than 20 centimeters in diameter are at higher risk of developing melanoma.
- Having unusual moles. Moles that are large with an irregular border are known as atypical nevi, also known as dysplastic nevi. They tend to run in families.
- Having many moles. Having more than 50 moles suggests a greater risk of melanoma and possibly breast cancer.
- Having a personal or family history of melanoma. If you've had melanoma before, there is a higher risk of getting melanoma again. Also, some types of atypical nevi lead to a genetic form of melanoma.
- Using tanning lamps or beds. Tanning lamps and beds release UV rays and can raise your risk of skin cancer.
Prevention
The following measures can help limit the growth of moles and the main complication of moles: melanoma.
Watch for changes
Become familiar with the location and pattern of your moles. Regularly look at your skin for changes that may signal melanoma. Do self-exams of the skin monthly. With the help of mirrors, do a head-to-toe check, including:
- Scalp.
- Palms and fingernails.
- Armpits.
- Chest.
- Legs.
- Feet, including the soles and between the toes.
- Genital area and between the buttocks.
Talk with your healthcare professional about your risk factors for melanoma and whether you need a professional skin exam regularly.
Protect your skin
Take measures to protect your skin from ultraviolet (UV) radiation, such as from the sun or tanning beds. UV radiation has been linked to a higher melanoma risk. And children who haven't been protected from sun exposure tend to grow more moles.
- Stay out of the sun during peak times. For many people in North America, the sun's rays are strongest between 10 a.m. and 2 p.m. Try to schedule outdoor activities for other times of the day, even on cloudy days or during the winter. When you are outdoors, seek shade or use an umbrella to protect yourself from the sun.
- Use sunscreen year-round. Apply sunscreen to dry skin about 15 minutes before going outdoors, even on cloudy days. Use a broad-spectrum, water-resistant sunscreen with an SPF of at least 30. Apply it generously and reapply every two hours — or more often if you're swimming or sweating.
- Wear protective clothing. Sunglasses, broad-brimmed hats, long sleeves and other clothing can protect you from damaging UV rays. You also might want to think about clothing that's made with fabric specially treated to block UV radiation.
- Don't use tanning lamps or beds. Tanning lamps and beds release UV rays that can raise your risk of skin cancer.
Diagnosis
Your healthcare professional can diagnose moles by looking at your skin. During a skin exam, your healthcare professional looks at your skin from head to toe. If your healthcare professional thinks that a mole may be cancerous, it is removed and sent to a lab for examination under a microscope. This is called a biopsy.
You might choose to make a skin exam a regular part of your preventive medical care. Talk with your healthcare professional about the schedule that's right for you.
Treatment
Most moles don't need treatment. If you're self-conscious about a mole, you could try makeup to help hide it. If you have a hair growing from a mole, you might try clipping it close to the skin's surface or plucking it. Anytime you cut or irritate a mole, keep the area clean. See your healthcare professional if a mole doesn't heal.
You also might talk with your dermatologist about surgically removing a mole if it bothers you or if you notice suspicious changes in it. Mole removal is a quick procedure that is typically done on an outpatient basis. During mole removal, your healthcare professional numbs the area around the mole and cuts it out, along with a margin of healthy skin if needed. The procedure may leave a permanent scar. People with Black skin are at increased risk of other surgical side effects, such as pigmentary changes where the cut is, and keloid scars, which are raised scars after an injury heals.
If you notice that a mole has grown back, see your healthcare professional promptly.
Preparing for an appointment
If you have a mole that concerns you, your healthcare professional typically can let you know if it's normal or needs to be studied more. Your healthcare professional may send you to a doctor who specializes in skin disorders, known as a dermatologist, for diagnosis and treatment.
It's a good idea to arrive for your appointment well-prepared. Here's some information to help you get ready.
What you can do
- List any changes you've noticed or any new symptoms you're having. Include any that may seem unrelated to the reason why you scheduled the appointment.
- Bring a list of all medicines, vitamins or supplements that you take.
- If you've had a melanoma or a mole removed in the past, note the location of the lesion and the date of removal. If you have the biopsy report, bring it with you.
- Don't wear makeup or opaque nail polish to your appointment. These products make it hard for your healthcare professional to do a thorough exam.
- List questions to ask your healthcare professional.
For moles, some basic questions to ask your healthcare professional include:
- Do you think this mole might be cancerous?
- What's the best course of action?
- How can I tell if a mole needs to be looked at?
- Can I keep more moles from growing?
- Do you have any brochures or other printed material that I can take home with me? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask questions during your appointment.
What to expect from your doctor
Your healthcare professional is likely to ask you several questions, such as:
- When did you first notice this mole?
- Have you always had it, or is it new?
- Have you noticed any changes in this mole, such as its color or shape?
- Have you had other moles surgically removed in the past? If so, do you know if they were unusual, known as atypical nevi, or malignant?
- Do you have a family history of atypical nevi, melanoma or other cancers?
- Have you had peeling sunburns or frequently been exposed to UV radiation, such as from tanning beds?



