High blood pressure (hypertension)
Overview
High blood pressure is a common condition that affects the body's arteries. It's also called hypertension. If you have high blood pressure, the force of the blood pushing against the artery walls is consistently too high. The heart has to work harder to pump blood.
Blood pressure is measured in millimeters of mercury (mm Hg). In general, hypertension is a blood pressure reading of 130/80 mm Hg or higher.
The American College of Cardiology and the American Heart Association divide blood pressure into four general categories. Ideal blood pressure is categorized as normal.
- Normal blood pressure. Blood pressure is lower than 120/80 mm Hg.
- Elevated blood pressure. The top number ranges from 120 to 129 mm Hg and the bottom number is below, not above, 80 mm Hg.
- Stage 1 hypertension. The top number ranges from 130 to 139 mm Hg or the bottom number is between 80 and 89 mm Hg.
- Stage 2 hypertension. The top number is 140 mm Hg or higher or the bottom number is 90 mm Hg or higher.
Blood pressure higher than 180/120 mm Hg is considered a hypertensive emergency or crisis. Seek emergency medical help for anyone with these blood pressure numbers.
Untreated, high blood pressure increases the risk of heart attack, stroke and other serious health problems. It's important to have your blood pressure checked at least every two years starting at age 18. Some people need more-frequent checks.
Healthy lifestyle habits —such as not smoking, exercising and eating well — can help prevent and treat high blood pressure. Some people need medicine to treat high blood pressure.
Symptoms
Most people with high blood pressure have no symptoms, even if blood pressure readings reach dangerously high levels. You can have high blood pressure for years without any symptoms.
A few people with high blood pressure may have:
- Headaches
- Shortness of breath
- Nosebleeds
However, these symptoms aren't specific. They usually don't occur until high blood pressure has reached a severe or life-threatening stage.
When to see a doctor
Blood pressure screening is an important part of general health care. How often you should get your blood pressure checked depends on your age and overall health.
Ask your provider for a blood pressure reading at least every two years starting at age 18. If you're age 40 or older, or you're 18 to 39 with a high risk of high blood pressure, ask for a blood pressure check every year.
Your care provider will likely recommend more-frequent readings if have high blood pressure or other risk factors for heart disease.
Children age 3 and older may have blood pressure measured as a part of their yearly checkups.
If you don't regularly see a care provider, you may be able to get a free blood pressure screening at a health resource fair or other locations in your community. Free blood pressure machines are also available in some stores and pharmacies. The accuracy of these machines depends on several things, such as a correct cuff size and proper use of the machines. Ask your health care provider for advice on using public blood pressure machines.
Causes
Blood pressure is determined by two things: the amount of blood the heart pumps and how hard it is for the blood to move through the arteries. The more blood the heart pumps and the narrower the arteries, the higher the blood pressure.
There are two main types of high blood pressure.
Primary hypertension, also called essential hypertension
For most adults, there's no identifiable cause of high blood pressure. This type of high blood pressure is called primary hypertension or essential hypertension. It tends to develop gradually over many years. Plaque buildup in the arteries, called atherosclerosis, increases the risk of high blood pressure.
Secondary hypertension
This type of high blood pressure is caused by an underlying condition. It tends to appear suddenly and cause higher blood pressure than does primary hypertension. Conditions and medicines that can lead to secondary hypertension include:
- Adrenal gland tumors
- Blood vessel problems present at birth, also called congenital heart defects
- Cough and cold medicines, some pain relievers, birth control pills, and other prescription drugs
- Illegal drugs, such as cocaine and amphetamines
- Kidney disease
- Obstructive sleep apnea
- Thyroid problems
Sometimes just getting a health checkup causes blood pressure to increase. This is called white coat hypertension.
Risk factors
High blood pressure has many risk factors, including:
- Age. The risk of high blood pressure increases with age. Until about age 64, high blood pressure is more common in men. Women are more likely to develop high blood pressure after age 65.
- Race. High blood pressure is particularly common among Black people. It develops at an earlier age in Black people than it does in white people.
- Family history. You're more likely to develop high blood pressure if you have a parent or sibling with the condition.
- Obesity or being overweight. Excess weight causes changes in the blood vessels, the kidneys and other parts of the body. These changes often increase blood pressure. Being overweight or having obesity also raises the risk of heart disease and its risk factors, such as high cholesterol.
- Lack of exercise. Not exercising can cause weight gain. Increased weight raises the risk of high blood pressure. People who are inactive also tend to have higher heart rates.
- Tobacco use or vaping. Smoking, chewing tobacco or vaping immediately raises blood pressure for a short while. Tobacco smoking injures blood vessel walls and speeds up the process of hardening of the arteries. If you smoke, ask your care provider for strategies to help you quit.
- Too much salt. A lot of salt — also called sodium — in the body can cause the body to retain fluid. This increases blood pressure.
- Low potassium levels. Potassium helps balance the amount of salt in the body's cells. A proper balance of potassium is important for good heart health. Low potassium levels may be due to a lack of potassium in the diet or certain health conditions, including dehydration.
- Drinking too much alcohol. Alcohol use has been linked with increased blood pressure, particularly in men.
- Stress. High levels of stress can lead to a temporary increase in blood pressure. Stress-related habits such as eating more, using tobacco or drinking alcohol can lead to further increases in blood pressure.
- Certain chronic conditions. Kidney disease, diabetes and sleep apnea are some of the conditions that can lead to high blood pressure.
- Pregnancy. Sometimes pregnancy causes high blood pressure.
High blood pressure is most common in adults. But kids can have high blood pressure too. High blood pressure in children may be caused by problems with the kidneys or heart. But for a growing number of kids, high blood pressure is due to lifestyle habits such as an unhealthy diet and lack of exercise.
Complications
The excessive pressure on the artery walls caused by high blood pressure can damage blood vessels and body organs. The higher the blood pressure and the longer it goes uncontrolled, the greater the damage.
Uncontrolled high blood pressure can lead to complications including:
- Heart attack or stroke. Hardening and thickening of the arteries due to high blood pressure or other factors can lead to a heart attack, stroke or other complications.
- Aneurysm. Increased blood pressure can cause a blood vessel to weaken and bulge, forming an aneurysm. If an aneurysm ruptures, it can be life-threatening.
- Heart failure. When you have high blood pressure, the heart has to work harder to pump blood. The strain causes the walls of the heart's pumping chamber to thicken. This condition is called left ventricular hypertrophy. Eventually, the heart can't pump enough blood to meet the body's needs, causing heart failure.
- Kidney problems. High blood pressure can cause the blood vessels in the kidneys to become narrow or weak. This can lead to kidney damage.
- Eye problems. Increased blood pressure can cause thickened, narrowed or torn blood vessels in the eyes. This can result in vision loss.
- Metabolic syndrome. This syndrome is a group of disorders of the body's metabolism. It involves the irregular breakdown of sugar, also called glucose. The syndrome includes increased waist size, high triglycerides, decreased high-density lipoprotein (HDL or "good") cholesterol, high blood pressure and high blood sugar levels. These conditions make you more likely to develop diabetes, heart disease and stroke.
- Changes with memory or understanding. Uncontrolled high blood pressure may affect the ability to think, remember and learn.
- Dementia. Narrowed or blocked arteries can limit blood flow to the brain. This can cause a certain type of dementia called vascular dementia. A stroke that interrupts blood flow to the brain also can cause vascular dementia.
Diagnosis
To diagnose high blood pressure, your health care provider examines you and asks questions about your medical history and any symptoms. Your provider listens to your heart using a device called a stethoscope.
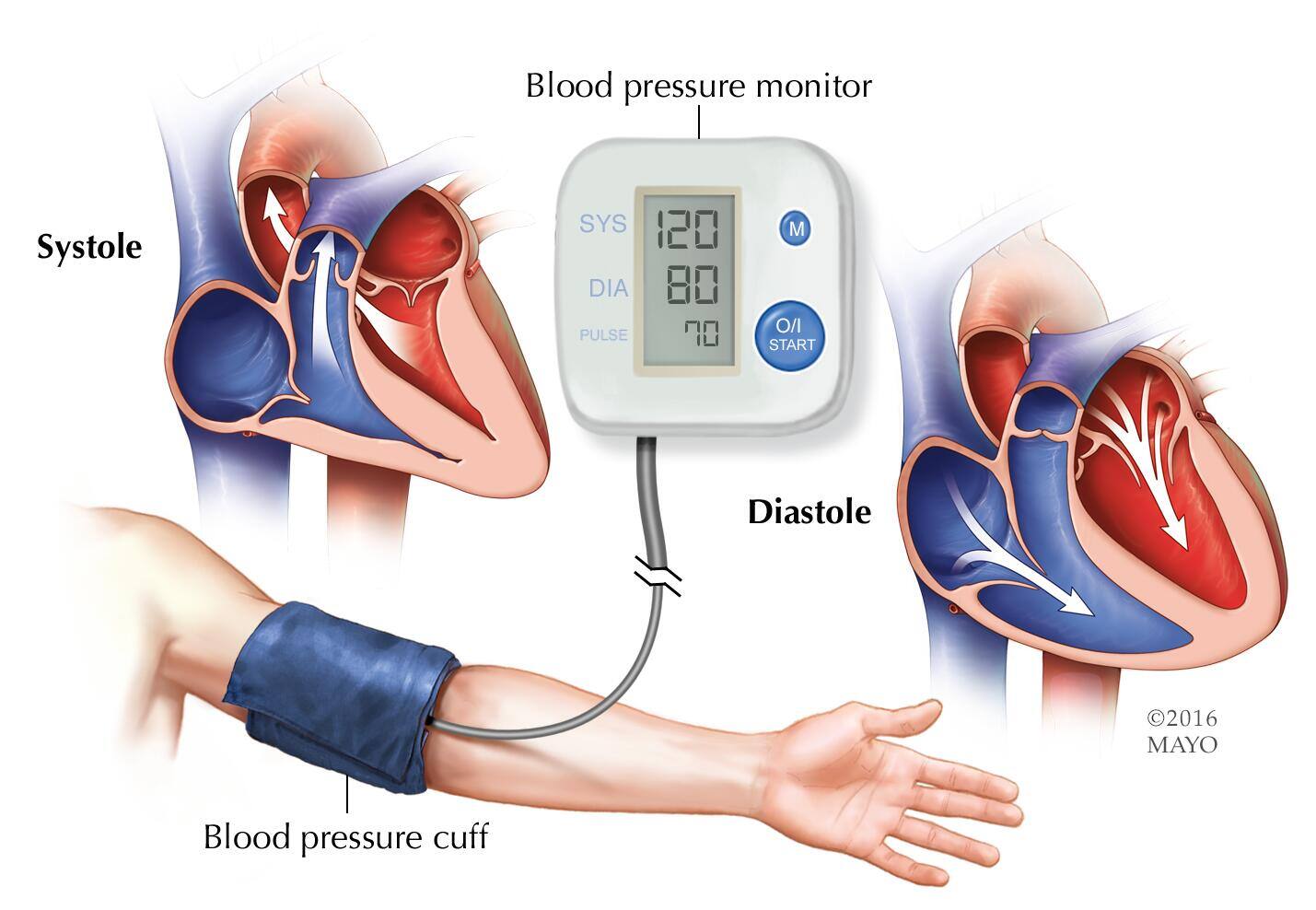
Your blood pressure is checked using a cuff, usually placed around your arm. It's important that the cuff fits. If it's too big or too small, blood pressure readings can vary. The cuff is inflated using a small hand pump or a machine.
The first time your blood pressure is checked, it should be measured in both arms to see if there's a difference. After that, the arm with the higher reading should be used.
Blood pressure is measured in millimeters of mercury (mm Hg). A blood pressure reading has two numbers.
- Top number, called systolic pressure. The first, or upper, number measures the pressure in the arteries when the heart beats.
- Bottom number, called diastolic pressure. The second, or lower, number measures the pressure in the arteries between heartbeats.
High blood pressure (hypertension) is diagnosed if the blood pressure reading is equal to or greater than 130/80 mm Hg. A diagnosis of high blood pressure is usually based on the average of two or more readings taken on separate occasions.
Blood pressure is grouped according to how high it is. This is called staging. Staging helps guide treatment.
- Stage 1 hypertension. The top number is between 130 and 139 mm Hg or the bottom number is between 80 and 89 mm Hg.
- Stage 2 hypertension. The top number is 140 mm Hg or higher or the bottom number is 90 mm Hg or higher.
Sometimes the bottom blood pressure reading is normal (less than 80 mm Hg) but the top number is high. This is called isolated systolic hypertension. It's a common type of high blood pressure in people older than 65.
Tests
If you are diagnosed with high blood pressure, your provider may recommend tests to check for a cause.
- Ambulatory monitoring. A longer blood pressure monitoring test may be done to check blood pressure at regular times over six or 24 hours. This is called ambulatory blood pressure monitoring. However, the devices used for the test aren't available in all medical centers. Check with your insurer to see if ambulatory blood pressure monitoring is a covered service.
- Lab tests. Blood and urine tests are done to check for conditions that can cause or worsen high blood pressure. For example, tests are done to check your cholesterol and blood sugar levels. You may also have lab tests to check your kidney, liver and thyroid function.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the heart's electrical activity. It can tell how fast or how slow the heart is beating. During an ECG, sensors called electrodes are attached to the chest and sometimes to the arms or legs. Wires connect the sensors to a machine, which prints or displays results.
- Echocardiogram. This noninvasive exam uses sound waves to create detailed images of the beating heart. It shows how blood moves through the heart and heart valves.
Taking your blood pressure at home
Your health care provider may ask you to regularly check your blood pressure at home. Home monitoring is a good way to keep track of your blood pressure. It helps your care providers know if your medicine is working or if your condition is getting worse.
Home blood pressure monitors are available at local stores and pharmacies.
For the most reliable blood pressure measurement, the American Heart Association recommends using a monitor with a cuff that goes around your upper arm, when available.
Devices that measure your blood pressure at your wrist or finger aren't recommended by the American Heart Association because they can provide less reliable results.
Treatment
Changing your lifestyle can help control and manage high blood pressure. Your health care provider may recommend that you make lifestyle changes including:
- Eating a heart-healthy diet with less salt
- Getting regular physical activity
- Maintaining a healthy weight or losing weight
- Limiting alcohol
- Not smoking
- Getting 7 to 9 hours of sleep daily
Sometimes lifestyle changes aren't enough to treat high blood pressure. If they don't help, your provider may recommend medicine to lower your blood pressure.
Medications
The type of medicine used to treat hypertension depends on your overall health and how high your blood pressure is. Two or more blood pressure drugs often work better than one. It can take some time to find the medicine or combination of medicines that works best for you.
When taking blood pressure medicine, it's important to know your goal blood pressure level. You should aim for a blood pressure treatment goal of less than 130/80 mm Hg if:
- You're a healthy adult age 65 or older
- You're a healthy adult younger than age 65 with a 10% or higher risk of developing cardiovascular disease in the next 10 years
- You have chronic kidney disease, diabetes or coronary artery disease
The ideal blood pressure goal can vary with age and health conditions, particularly if you're older than age 65.
Medicines used to treat high blood pressure include:
-
Water pills (diuretics). These drugs help remove sodium and water from the body. They are often the first medicines used to treat high blood pressure.
There are different classes of diuretics, including thiazide, loop and potassium sparing. Which one your provider recommends depends on your blood pressure measurements and other health conditions, such as kidney disease or heart failure. Diuretics commonly used to treat blood pressure include chlorthalidone, hydrochlorothiazide (Microzide) and others.
A common side effect of diuretics is increased urination. Urinating a lot can reduce potassium levels. A good balance of potassium is necessary to help the heart beat correctly. If you have low potassium (hypokalemia), your provider may recommend a potassium-sparing diuretic that contains triamterene.
- Angiotensin-converting enzyme (ACE) inhibitors. These drugs help relax blood vessels. They block the formation of a natural chemical that narrows blood vessels. Examples include lisinopril (Prinivil, Zestril), benazepril (Lotensin), captopril and others.
- Angiotensin II receptor blockers (ARBs). These drugs also relax blood vessels. They block the action, not the formation, of a natural chemical that narrows blood vessels. ARBs include candesartan (Atacand), losartan (Cozaar) and others.
-
Calcium channel blockers. These drugs help relax the muscles of the blood vessels. Some slow your heart rate. They include amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and others. Calcium channel blockers may work better for older people and Black people than do ACE inhibitors alone.
Don't eat or drink grapefruit products when taking calcium channel blockers. Grapefruit increases blood levels of certain calcium channel blockers, which can be dangerous. Talk to your provider or pharmacist if you're concerned about interactions.
Other medicines sometimes used to treat high blood pressure
If you're having trouble reaching your blood pressure goal with combinations of the above medicines, your provider may prescribe:
- Alpha blockers. These medicines reduce nerve signals to blood vessels. They help lower the effects of natural chemicals that narrow blood vessels. Alpha blockers include doxazosin (Cardura), prazosin (Minipress) and others.
- Alpha-beta blockers. Alpha-beta blockers block nerve signals to blood vessels and slow the heartbeat. They reduce the amount of blood that must be pumped through the vessels. Alpha-beta blockers include carvedilol (Coreg) and labetalol (Trandate).
-
Beta blockers. These medicines reduce the workload on the heart and widen the blood vessels. This helps the heart beat slower and with less force. Beta blockers include atenolol (Tenormin), metoprolol (Lopressor, Toprol-XL, Kapspargo sprinkle) and others.
Beta blockers aren't usually recommended as the only medicine prescribed. They may work best when combined with other blood pressure drugs.
- Aldosterone antagonists. These drugs may be used to treat resistant hypertension. They block the effect of a natural chemical that can lead to salt and fluid buildup in the body. Examples are spironolactone (Aldactone) and eplerenone (Inspra).
-
Renin inhibitors. Aliskiren (Tekturna) slows the production of renin, an enzyme produced by the kidneys that starts a chain of chemical steps that increases blood pressure.
Due to a risk of serious complications, including stroke, you shouldn't take aliskiren with ACE inhibitors or ARBs.
- Vasodilators. These medicines stop the muscles in the artery walls from tightening. This prevents the arteries from narrowing. Examples include hydralazine and minoxidil.
- Central-acting agents. These medicines prevent the brain from telling the nervous system to increase the heart rate and narrow the blood vessels. Examples include clonidine (Catapres, Kapvay), guanfacine (Intuniv) and methyldopa.
Always take blood pressure medicines as prescribed. Never skip a dose or abruptly stop taking blood pressure medicines. Suddenly stopping certain ones, such as beta blockers, can cause a sharp increase in blood pressure called rebound hypertension.
If you skip doses because of cost, side effects or forgetfulness, talk to your care provider about solutions. Don't change your treatment without your provider's guidance.
Treating resistant hypertension
You may have resistant hypertension if:
- You take at least three different blood pressure drugs, including a diuretic. But your blood pressure remains stubbornly high.
- You're taking four different medicines to control high blood pressure. Your care provider should check for a possible second cause of the high blood pressure.
Having resistant hypertension doesn't mean your blood pressure will never get lower. If you and your provider can determine the cause, a more effective treatment plan can be created.
Treating resistant hypertension may involve many steps, including:
- Changing blood pressure medicines to find the best combination and dosage.
- Reviewing all your medicines, including those bought without a prescription.
- Checking blood pressure at home to see if medical appointments cause high blood pressure. This is called white coat hypertension.
- Eating healthy, managing weight and making other recommended lifestyle changes.
High blood pressure during pregnancy
If you have high blood pressure and are pregnant, discuss with your care providers how to control blood pressure during your pregnancy.
Potential future treatments
Researchers have been studying the use of heat to destroy specific nerves in the kidney that may play a role in resistant hypertension. The method is called renal denervation. Early studies showed some benefit. But more-robust studies found that it doesn't significantly lower blood pressure in people with resistant hypertension. More research is underway to determine what role, if any, this therapy may have in treating hypertension.
Self care
A commitment to a healthy lifestyle can help prevent and manage high blood pressure. Try these heart-healthy strategies:
- Eat healthy foods. Eat a healthy diet. Try the Dietary Approaches to Stop Hypertension (DASH) diet. Choose fruits, vegetables, whole grains, poultry, fish and low-fat dairy foods. Get plenty of potassium from natural sources, which can help lower blood pressure. Eat less saturated fat and trans fat.
- Use less salt. Processed meats, canned foods, commercial soups, frozen dinners and certain breads can be hidden sources of salt. Check food labels for the sodium content. Limit foods and beverages that are high in sodium. A sodium intake of 1,500 mg a day or less is considered ideal for most adults. But ask your provider what's best for you.
- Limit alcohol. Even if you're healthy, alcohol can raise your blood pressure. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women, and up to two drinks a day for men. One drink equals 12 ounces of beer, 5 ounces of wine or 1.5 ounces of 80-proof liquor.
- Don't smoke. Tobacco injures blood vessel walls and speeds up the process of hardening of the arteries. If you smoke, ask your care provider for strategies to help you quit.
- Maintain a healthy weight. If you're overweight or have obesity, losing weight can help control blood pressure and lower the risk of complications. Ask your health care provider what weight is best for you. In general, blood pressure drops by about 1 mm Hg with every 2.2 pounds (1 kilogram) of weight lost. In people with high blood pressure, the drop in blood pressure may be even more significant per kilogram of weight lost.
-
Get more exercise. Regular exercise keeps the body healthy. It can lower blood pressure, ease stress, manage weight and reduce the risk of chronic health conditions. Aim to get at least 150 minutes a week of moderate aerobic activity or 75 minutes a week of vigorous aerobic activity, or a combination of the two.
If you have high blood pressure, consistent moderate- to high-intensity workouts can lower your top blood pressure reading by about 11 mm Hg and the bottom number by about 5 mm Hg.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily. Kids often need more. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to your provider about strategies that might help.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce stress.
- Try slow, deep breathing. Practice taking deep, slow breaths to help relax. Some research shows that slow, paced breathing (5 to 7 deep breaths per minute) combined with mindfulness techniques can reduce blood pressure. There are devices available to promote slow, deep breathing. According to the American Heart Association, device-guided breathing may be a reasonable nondrug option for lowering blood pressure. It may be a good option if you have anxiety with high blood pressure or can't tolerate standard treatments.
Alternative medicine
Diet and exercise are the best ways to lower blood pressure. But some supplements are promoted as heart healthy. These supplements include:
- Fiber, such as blond psyllium and wheat bran
- Minerals, such as magnesium, calcium and potassium
- Folic acid
- Supplements or products that increase nitric oxide or widen blood vessels — called vasodilators — such as cocoa, coenzyme Q10, L-arginine and garlic
- Omega-3 fatty acids, found in fatty fish, high-dose fish oil supplements and flaxseed
Researchers are also studying whether vitamin D can reduce blood pressure, but evidence is conflicting. More research is needed.
Talk to your care provider before adding any supplements to your blood pressure treatment. Some can interact with medicines, causing harmful side effects that could be life-threatening.
Deep breathing or mindfulness are alternative medicine techniques that can help you relax. These practices may temporarily reduce blood pressure.
Coping and support
High blood pressure isn't something that you can treat and then ignore. It's a condition that requires regular health checkups. Some things you can do to help manage the condition are:
- Take medicines as directed. If side effects or costs pose problems, ask your provider about other options. Don't stop taking your medicines without first talking to a care provider.
- Schedule regular health checkups. It takes a team effort to treat high blood pressure successfully. Work with your provider to bring your blood pressure to a safe level and keep it there. Know your goal blood pressure level.
- Choose healthy habits. Eat healthy foods, lose excess weight and get regular physical activity. Limit alcohol. If you smoke, quit.
- Manage stress. Say no to extra tasks, release negative thoughts, and remain patient and optimistic.
- Ask for help. Sticking to lifestyle changes can be difficult, especially if you don't see or feel any symptoms of high blood pressure. It may help to ask your friends and family to help you meet your goals.
- Join a support group. You may find that talking about any concerns with others in similar situations can help.
Preparing for your appointment
If you think you may have high blood pressure, make an appointment with your health care provider for a blood pressure test. You might want to wear a short-sleeved shirt to your appointment so it's easier to place the blood pressure cuff around your arm.
No special preparations are necessary for a blood pressure test. To get an accurate reading, avoid caffeine, exercise and tobacco for at least 30 minutes before the test.
Because some medicines can raise blood pressure, bring a list of all medicines, vitamins and other supplements you take and their doses to your medical appointment. Don't stop taking any medicines without your provider's advice.
Appointments can be brief. Because there's often a lot to discuss, it's a good idea to be prepared for your appointment. Here's some information to help you get ready.
What you can do
- Write down any symptoms that you're having. High blood pressure rarely has symptoms, but it's a risk factor for heart disease. Let your care provider know if you have symptoms such as chest pains or shortness of breath. Doing so can help your provider decide how aggressively to treat your high blood pressure.
- Write down important medical information, including a family history of high blood pressure, high cholesterol, heart disease, stroke, kidney disease or diabetes, and any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking. Include dosages.
- Take a family member or friend along, if possible. Sometimes it can be difficult to remember all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Be prepared to discuss your diet and exercise habits. If you don't already follow a diet or exercise routine, be ready to talk to your care provider about any challenges you might face in getting started.
- Write down questions to ask your provider.
Preparing a list of questions can help you and your provider make the most of your time together. List your questions from most important to least important in case time runs out. For high blood pressure, some basic questions to ask your provider include:
- What kinds of tests will I need?
- What is my blood pressure goal?
- Do I need any medicines?
- Is there a generic alternative to the medicine you're prescribing for me?
- What foods should I eat or avoid?
- What's an appropriate level of physical activity?
- How often do I need to schedule appointments to check my blood pressure?
- Should I monitor my blood pressure at home?
- I have other health conditions. How can I best manage them together?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask any other questions that you might have.
What to expect from your doctor
Your health care provider is likely to ask you questions. Being ready to answer them may reserve time to go over any points you want to spend more time on. Your provider may ask:
- Do you have a family history of high cholesterol, high blood pressure or heart disease?
- What are your diet and exercise habits like?
- Do you drink alcohol? How many drinks do you have in a week?
- Do you smoke?
- When did you last have your blood pressure checked? What was the result?
What you can do in the meantime
It's never too early to make healthy lifestyle changes, such as quitting smoking, eating healthy foods and getting more exercise. These are the main ways to protect yourself against high blood pressure and its complications, including heart attack and stroke.



