Gastrointestinal bleeding
Symptoms
Symptoms of GI bleeding can be easy to see, called overt, or not so obvious, known as occult. Symptoms depend on the rate of bleeding as well as the location of the bleed, which can be anywhere on the GI tract, from where it starts — the mouth — to where it ends — the anus.
Overt bleeding might show up as:
- Vomiting blood, which might be red or might be dark brown and look like coffee grounds.
- Black, tarry stool.
- Rectal bleeding, usually in or with stool.
With occult bleeding, you might have:
- Lightheadedness.
- Difficulty breathing.
- Fainting.
- Chest pain.
- Abdominal pain.
Symptoms of shock
If your bleeding starts suddenly and gets worse quickly, you could go into shock. Symptoms of shock include:
- Weakness or fatigue.
- Dizziness or fainting.
- Cool, clammy, pale skin.
- Nausea or vomiting.
- Not urinating or urinating a little at a time.
- A gray or bluish tinge to lips or fingernails.
- Changes in mental status or behavior, such as anxiousness or agitation.
- Unconsciousness.
- Rapid pulse.
- Rapid breathing.
- Drop in blood pressure.
- Enlarged pupils.
When to see a doctor
If you have symptoms of shock, you or someone else should call 911 or your local emergency medical number. If you're vomiting blood, see blood in your stools or have black, tarry stools, seek immediate medical care. If you notice any symptoms of GI bleeding, make an appointment with your doctor.
Causes
Gastrointestinal bleeding can happen either in the upper or lower gastrointestinal tract.
Upper GI bleeding
Causes of upper GI bleeding can include:
- Peptic ulcer. This is the most common cause of upper GI bleeding. Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper part of your small intestine. Stomach acid, either from bacteria or use of anti-inflammatory medicines, such as ibuprofen or aspirin, damages the lining, causing sores to form.
- Tears in the lining of the tube that connects your throat to your stomach, called the esophagus. Known as Mallory-Weiss tears, they can cause a lot of bleeding. These are most common in people who drink alcohol to excess, leading to retching and vomiting.
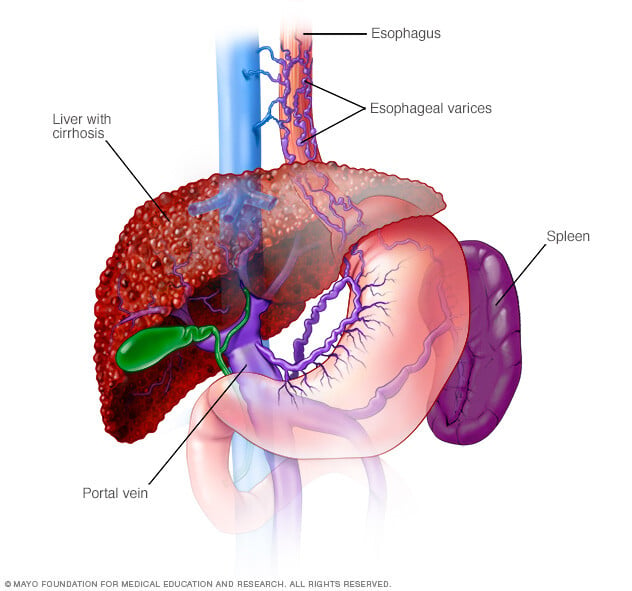
- Enlarged veins in the esophagus, called esophageal varices. This condition occurs most often in people with serious liver disease, most commonly due to excessive alcohol use.
- Portal hypertensive gastropathy. This condition occurs most often in people with serious liver disease, most commonly due to excessive alcohol use.
- Esophagitis. This inflammation of the esophagus is most often caused by gastroesophageal reflux disease (GERD).
- Abnormal blood vessels. At times abnormal blood vessels, small bleeding arteries and veins may lead to bleeding.
- Hiatal hernia. Large hiatal hernias may be associated with erosions in the stomach, leading to bleeding.
- Growths. Though rare, upper GI bleeding can be caused by cancerous or noncancerous growths in the upper digestive tract.
Lower GI bleeding
Causes can include:
- Diverticular disease. This involves the development of small, bulging pouches in the digestive tract, called diverticulosis. If one or more of the pouches become inflamed or infected, it's called diverticulitis.
- Inflammatory bowel disease (IBD). This includes ulcerative colitis, which causes swollen tissues and sores in the colon and rectum. Another form of IBD, Crohn's disease, involves swollen, irritated tissues in the lining of the digestive tract.
- Proctitis. Inflammation of the lining of the rectum can cause rectal bleeding.
- Tumors. Noncancerous or cancerous tumors of the esophagus, stomach, colon or rectum can weaken the lining of the digestive tract and cause bleeding.
- Colon polyps. Small clumps of cells that form on the lining of your colon can cause bleeding. Most are harmless, but some might be cancerous or can become cancerous if not removed.
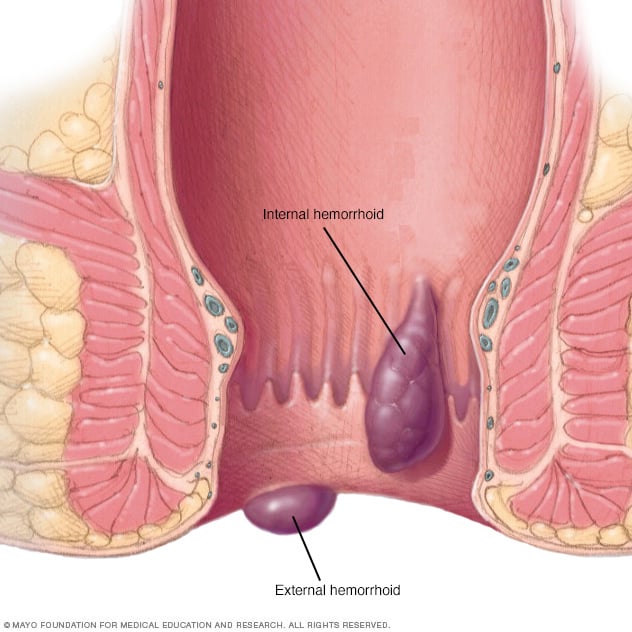
- Hemorrhoids. These are swollen veins in your anus or lower rectum, such as varicose veins.
- Anal fissures. An anal fissure is a small tear in the thin, moist tissue that lines the anus.
Complications
A gastrointestinal bleed can cause:
- Anemia.
- Shock.
- Death.
Prevention
To help prevent a GI bleed:
- Limit your use of nonsteroidal anti-inflammatory drugs.
- Limit your use of alcohol.
- If you smoke, quit.
- If you have GERD, follow your health care team's instructions for treating it.
Diagnosis
To find the cause of gastrointestinal bleeding, a health care professional will first take your medical history, including a history of previous bleeding, and do a physical exam. Tests also may be ordered, such as:
- Blood tests. You may need a complete blood count, a test to see how fast your blood clots, a platelet count and liver function tests.
- Stool tests. Analyzing your stool can help determine the cause of occult bleeding.
- Nasogastric lavage. A tube is passed through your nose into the stomach to remove stomach contents. This might help find the source of the bleeding.
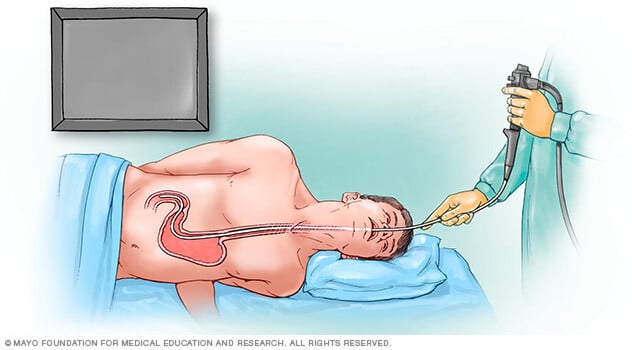
- Upper endoscopy. An upper endoscopy is a procedure that uses a camera to view the upper digestive system. The camera is attached to a long, thin tube, called an endoscope, and passed down the throat to examine the upper gastrointestinal tract.
- Colonoscopy. During a colonoscopy, a long, flexible tube is inserted into the rectum. A tiny video camera at the tip of the tube allows the doctor to view the inside of the entire large intestine and rectum.
- Capsule endoscopy. In this procedure, you swallow a vitamin-size capsule with a tiny camera inside. The capsule travels through your digestive tract taking thousands of pictures that are sent to a recorder you wear on a belt around your waist.
- Flexible sigmoidoscopy. A tube with a light and camera is placed in the rectum to look at the rectum and the last part of the large intestine, known as the sigmoid colon.
- Balloon-assisted enteroscopy. A specialized scope inspects parts of the small intestine that other tests using an endoscope can't reach. Sometimes, the source of bleeding can be controlled or treated during this test.
- Angiography. A contrast dye is injected into an artery, and a series of X-rays are taken to look for and treat bleeding vessels or other issues.
- Imaging tests. A variety of other imaging tests, such as a CT scan of the belly, might be used to find the source of the bleed.
If your GI bleeding is severe, and noninvasive tests can't find the source, you might need surgery so that doctors can view the entire small intestine. Fortunately, this is rare.
Treatment
GI bleeding often stops on its own. If it doesn't, treatment depends on where the bleed is from. In many cases, bleeding can be treated with medicine or a procedure during a test. For example, it's sometimes possible to treat a bleeding peptic ulcer during an upper endoscopy or to remove polyps during a colonoscopy.
If you have an upper GI bleed, you will be given an IV drug known as a proton pump inhibitor (PPI) to suppress stomach acid production. Once the source of the bleeding is identified, your doctor will determine whether you need to continue taking a PPI.
Depending on the amount of blood loss and whether you continue to bleed, you might need fluids through a needle (IV) and, possibly, blood transfusions. If you take blood-thinning medicines, including aspirin or nonsteroidal anti-inflammatory medications, you might need to stop.
Preparing for an appointment
If your bleeding is not severe, you might start by seeing your doctor or other general health care professional. Or you might be referred immediately to a specialist in gastrointestinal disorders, called a gastroenterologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment and when they began.
- All medicines, vitamins or other supplements you take, including doses.
- History of digestive disease you've been diagnosed with, such as GERD, peptic ulcers or IBD.
- Questions to ask during your appointment.
Take a family member or friend along, if possible, to help you remember the information you're given.
For gastrointestinal bleeding, basic questions to ask include:
- I'm not seeing blood, so why do you suspect a GI bleed?
- What's likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What's the best course of action?
- What are the alternatives to the primary approach you're suggesting?
- I have other health conditions. How can I best manage them while my bleeding is treated?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
You'll likely be asked a few questions, such as:
- Have your symptoms been constant? Or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do you take nonsteroidal anti-inflammatory medicine, either nonprescription or prescribed, or do you take aspirin?
- Do you drink alcohol?



