Fetal macrosomia
Overview
The term "fetal macrosomia" is used to describe a newborn who's much larger than average.
A baby who is diagnosed as having fetal macrosomia weighs more than 8 pounds, 13 ounces (4,000 grams), regardless of his or her gestational age. About 9% of babies worldwide weigh more than 8 pounds, 13 ounces.
Risks associated with fetal macrosomia increase greatly when birth weight is more than 9 pounds, 15 ounces (4,500 grams).
Fetal macrosomia may complicate vaginal delivery and can put the baby at risk of injury during birth. Fetal macrosomia also puts the baby at increased risk of health problems after birth.
Symptoms
Fetal macrosomia can be difficult to detect and diagnose during pregnancy. Signs and symptoms include:
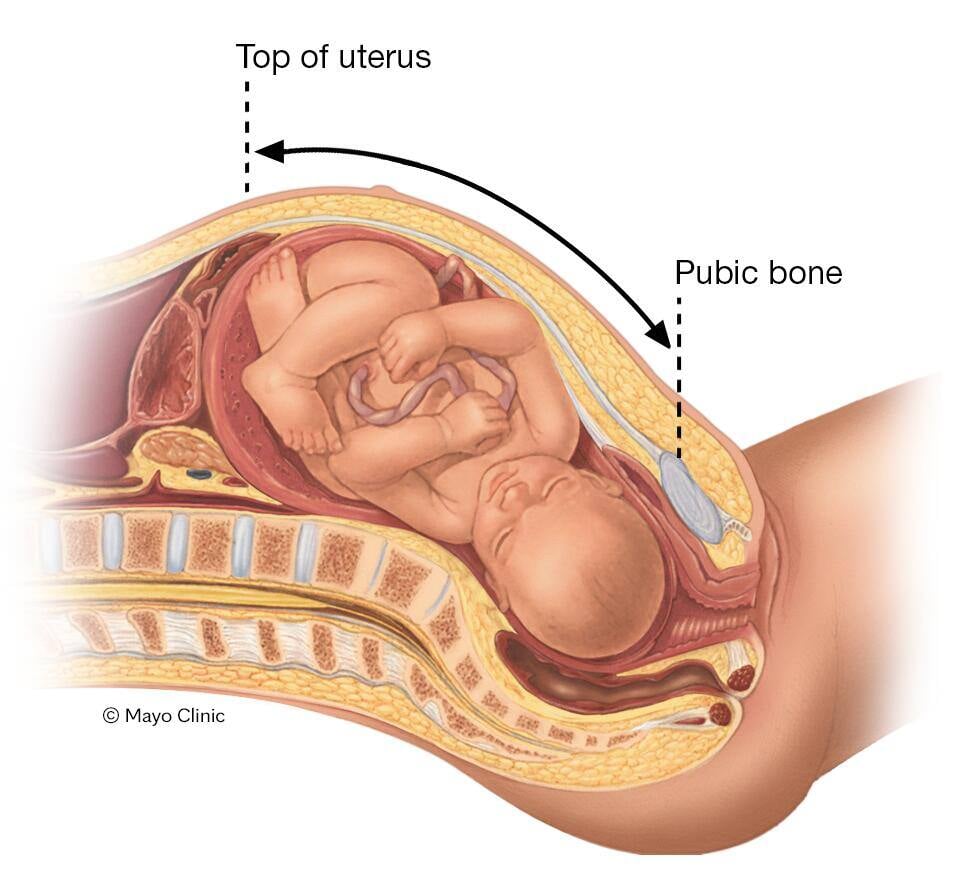
- Large fundal height. During prenatal visits, your health care provider might measure your fundal height — the distance from the top of your uterus to your pubic bone. A larger than expected fundal height could be a sign of fetal macrosomia.
-
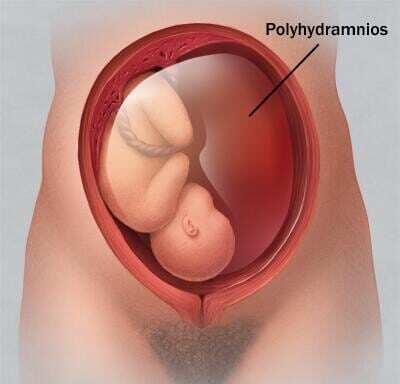
Excessive amniotic fluid (polyhydramnios). Having too much amniotic fluid — the fluid that surrounds and protects a baby during pregnancy — might be a sign that your baby is larger than average.
The amount of amniotic fluid reflects your baby's urine output, and a larger baby produces more urine. Some conditions that cause a baby to be larger might also increase his or her urine output.
Causes
Genetic factors and maternal conditions such as obesity or diabetes can cause fetal macrosomia. Rarely, a baby might have a medical condition that makes him or her grow faster and larger.
Sometimes it's unknown what causes a baby to be larger than average.
Risk factors
Many factors might increase the risk of fetal macrosomia — some you can control, but others you can't.
For example:
-
Maternal diabetes. Fetal macrosomia is more likely if you had diabetes before pregnancy (pre-gestational diabetes) or if you develop diabetes during pregnancy (gestational diabetes).
If your diabetes isn't well controlled, your baby is likely to have larger shoulders and greater amounts of body fat than would a baby whose mother doesn't have diabetes.
- A history of fetal macrosomia. If you've previously given birth to a large baby, you're at increased risk of having another large baby. Also, if you weighed more than 8 pounds, 13 ounces at birth, you're more likely to have a large baby.
- Maternal obesity. Fetal macrosomia is more likely if you're obese.
- Excessive weight gain during pregnancy. Gaining too much weight during pregnancy increases the risk of fetal macrosomia.
- Previous pregnancies. The risk of fetal macrosomia increases with each pregnancy. Up to the fifth pregnancy, the average birth weight for each successive pregnancy typically increases by up to about 4 ounces (113 grams).
- Having a boy. Male infants typically weigh slightly more than female infants. Most babies who weigh more than 9 pounds, 15 ounces (4,500 grams) are male.
- Overdue pregnancy. If your pregnancy continues by more than two weeks past your due date, your baby is at increased risk of fetal macrosomia.
- Maternal age. Women older than 35 are more likely to have a baby diagnosed with fetal macrosomia.
Fetal macrosomia is more likely to be a result of maternal diabetes, obesity or weight gain during pregnancy than other causes. If these risk factors aren't present and fetal macrosomia is suspected, it's possible that your baby might have a rare medical condition that affects fetal growth.
If a rare medical condition is suspected, your health care provider might recommend prenatal diagnostic tests and perhaps a visit with a genetic counselor, depending on the test results.
Complications
Fetal macrosomia poses health risks for you and your baby — both during pregnancy and after childbirth.
Maternal risks
Possible maternal complications of fetal macrosomia might include:
- Labor problems. Fetal macrosomia can cause a baby to become wedged in the birth canal (shoulder dystocia), sustain birth injuries, or require the use of forceps or a vacuum device during delivery (operative vaginal delivery). Sometimes a C-section is needed.
- Genital tract lacerations. During childbirth, fetal macrosomia can cause a baby to injure the birth canal — such as by tearing vaginal tissues and the muscles between the vagina and the anus (perineal muscles).
- Bleeding after delivery. Fetal macrosomia increases the risk that your uterine muscles won't properly contract after you give birth (uterine atony). This can lead to potentially serious bleeding after delivery.
- Uterine rupture. If you've had a prior C-section or major uterine surgery, fetal macrosomia increases the risk of uterine rupture during labor — a rare but serious complication in which the uterus tears open along the scar line from the C-section or other uterine surgery. An emergency C-section is needed to prevent life-threatening complications.
Newborn and childhood risks
Possible complications of fetal macrosomia for your baby might include:
- Lower than normal blood sugar level. A baby diagnosed with fetal macrosomia is more likely to be born with a blood sugar level that's lower than normal.
- Childhood obesity. Research suggests that the risk of childhood obesity increases as birth weight increases.
-
Metabolic syndrome. If your baby is diagnosed with fetal macrosomia, he or she is at risk of developing metabolic syndrome during childhood.
Metabolic syndrome is a cluster of conditions — increased blood pressure, a high blood sugar level, excess body fat around the waist and abnormal cholesterol levels — that occur together, increasing the risk of heart disease, stroke and diabetes.
Further research is needed to determine whether these effects might increase the risk of adult diabetes, obesity and heart disease.
Prevention
You might not be able to prevent fetal macrosomia, but you can promote a healthy pregnancy. Research shows that exercising during pregnancy and eating a low-glycemic diet can reduce the risk of macrosomia.
For example:
- Schedule a preconception appointment. If you're considering pregnancy, talk with your health care provider. If you're obese, you might also be referred to another health care provider — such as a registered dietitian or an obesity specialist — who can help you reach a healthy weight before pregnancy.
- Monitor your weight. Gaining a healthy amount of weight during pregnancy — often 25 to 35 pounds (about 11 to 16 kilograms) if you have a normal pre-pregnancy weight — supports your baby's growth and development. Women who weigh more when they get pregnant will have lower recommended pregnancy weight gain. Work with your health care provider to determine what's right for you.
- Manage diabetes. If you had diabetes before pregnancy or if you develop gestational diabetes, work with your health care provider to manage the condition. Controlling your blood sugar level is the best way to prevent complications, including fetal macrosomia.
- Be active. Follow your health care provider's recommendations for physical activity.
Diagnosis
Fetal macrosomia can't be diagnosed until after the baby is born and weighed.
However, if you have risk factors for fetal macrosomia, your health care provider will likely use tests to monitor your baby's health and development while you're pregnant, such as:
-
Ultrasound. Toward the end of your third trimester, your health care provider or another member of your health care team might do an ultrasound to take measurements of parts of your baby's body, such as the head, abdomen and femur. Your health care provider will then plug these measurements into a formula to estimate your baby's weight.
However, the accuracy of ultrasound for predicting fetal macrosomia has been unreliable.
-
Antenatal testing. If your health care provider suspects fetal macrosomia, he or she might perform antenatal testing, such as a nonstress test or a fetal biophysical profile, to monitor your baby's well-being.
A nonstress test measures the baby's heart rate in response to his or her own movements. A fetal biophysical profile combines nonstress testing with ultrasound to monitor your baby's movement, tone, breathing and volume of amniotic fluid.
If your baby's excess growth is thought to be the result of a maternal condition, your health care provider might recommend antenatal testing — starting as early as week 32 of pregnancy.
Note that macrosomia alone is not a reason for antenatal testing to monitor your baby's well-being.
Before your baby is born, you might also consider consulting a pediatrician who has expertise in treating babies diagnosed with fetal macrosomia.
Treatment
When it's time for your baby to be born, a vaginal delivery won't necessarily be out of the question. Your health care provider will discuss options as well as risks and benefits. He or she will monitor your labor closely for possible signs of a complicated vaginal delivery.
Inducing labor — stimulating uterine contractions before labor begins on its own — isn't generally recommended. Research suggests that labor induction doesn't reduce the risk of complications related to fetal macrosomia and might increase the need for a C-section.
Your health care provider might recommend a C-section if:
- You have diabetes. If you had diabetes before pregnancy or you develop gestational diabetes and your health care provider estimates that your baby weighs 9 pounds, 15 ounces (4,500 grams) or more, a C-section might be the safest way to deliver your baby.
- Your baby weighs 11 pounds or more and you don't have a history of maternal diabetes. If you don't have pre-gestational or gestational diabetes and your health care provider estimates that your baby weighs 11 pounds (5,000 grams) or more, a C-section might be recommended.
- You delivered a baby whose shoulder got stuck behind your pelvic bone (shoulder dystocia). If you've delivered one baby with shoulder dystocia, you're at increased risk of the problem occurring again. A C-section might be recommended to avoid the risks associated with shoulder dystocia, such as a fractured collarbone.
If your health care provider recommends an elective C-section, be sure to discuss the risks and benefits.
After your baby is born, he or she will likely be examined for signs of birth injuries, abnormally low blood sugar (hypoglycemia) and a blood disorder that affects the red blood cell count (polycythemia). He or she might need special care in the hospital's neonatal intensive care unit.
Keep in mind that your baby might be at risk of childhood obesity and insulin resistance and should be monitored for these conditions during future checkups.
Also, if you haven't previously been diagnosed with diabetes and your health care provider is concerned about the possibility of diabetes, you may be tested for the condition. During future pregnancies, you'll be closely monitored for signs and symptoms of gestational diabetes — a type of diabetes that develops during pregnancy.
Coping and support
If your health care provider suspects fetal macrosomia during your pregnancy, you might feel anxious about childbirth and your baby's health — and worrying can make it hard to take care of yourself.
Consult your health care provider about what you can do to relieve stress and promote your baby's health. Also consider seeking information and support from women who've had babies diagnosed with fetal macrosomia.
Preparing for your appointment
If you have risk factors for fetal macrosomia, the topic is likely to come up at routine prenatal appointments.
Below are some basic questions to ask your health care provider about fetal macrosomia:
- What is likely causing the condition?
- What kinds of tests do I need?
- What needs to be done now?
- Do I need to follow any restrictions?
- How will fetal macrosomia affect my baby?
- Will I need to have a C-section?
- Will my baby need tests or special care after he or she is born?
In addition to the questions you've prepared, don't hesitate to ask other questions during your appointment.