Cholecystitis
Overview
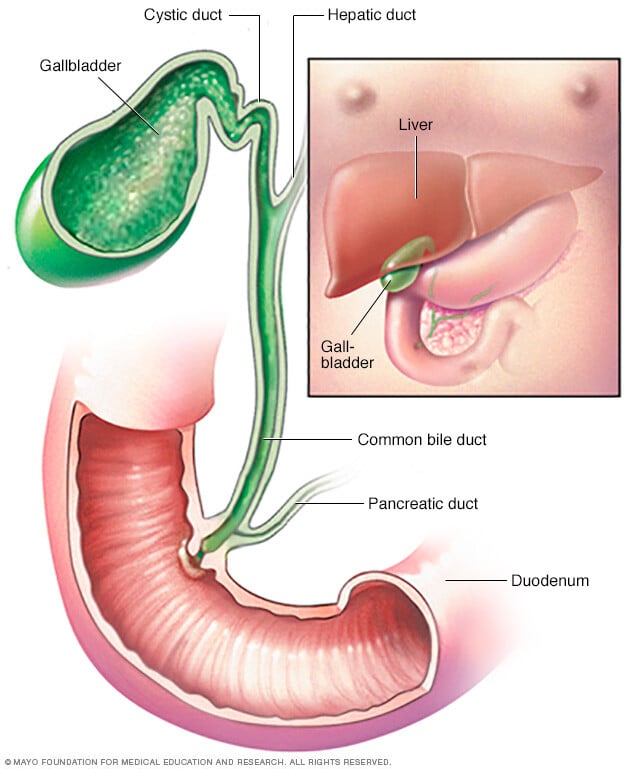
Cholecystitis (ko-luh-sis-TIE-tis) is inflammation of the gallbladder. The gallbladder is a small, pear-shaped organ on the right side of the belly (abdomen), beneath the liver. The gallbladder holds a digestive fluid (bile) that's released into the small intestine.
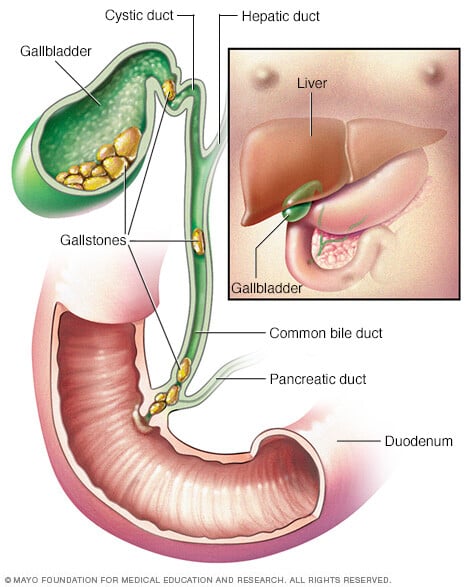
In most cases, gallstones blocking the tube leading out of the gallbladder cause cholecystitis. This results in a bile buildup that can cause inflammation. Other causes of cholecystitis include bile duct problems, tumors, serious illness and certain infections.
If left untreated, cholecystitis can lead to severe, sometimes life-threatening complications, such as a gallbladder rupture. Treatment for cholecystitis often involves surgery to remove the gallbladder.
Symptoms
Symptoms of cholecystitis may include:
- Severe pain in your upper right or center abdomen
- Pain that spreads to your right shoulder or back
- Tenderness over your abdomen when it's touched
- Nausea
- Vomiting
- Fever
Cholecystitis symptoms often occur after a meal, particularly a large or fatty one.
When to see a doctor
Make an appointment with your health care provider if you have symptoms that worry you. If your abdominal pain is so severe that you can't sit still or get comfortable, have someone drive you to the emergency room.
Causes
Cholecystitis is when your gallbladder is inflamed. Gallbladder inflammation can be caused by:
- Gallstones. Most often, cholecystitis is the result of hard particles that develop in your gallbladder (gallstones). Gallstones can block the tube (cystic duct) through which bile flows when it leaves the gallbladder. Bile builds up in the gallbladder, causing inflammation.
- Tumor. A tumor may prevent bile from draining out of your gallbladder properly. This causes bile buildup that can lead to cholecystitis.
- Bile duct blockage. Stones or thickened bile and tiny particles (sludge) can block the bile duct and lead to cholecystitis. Kinking or scarring of the bile ducts can also cause blockage.
- Infection. AIDS and certain viral infections can trigger gallbladder inflammation.
- Severe illness. Very severe illness can damage blood vessels and decrease blood flow to the gallbladder, leading to cholecystitis.
Risk factors
Having gallstones is the main risk factor for developing cholecystitis.
Complications
If untreated, cholecystitis can lead to a number of serious complications, including:
- Infection within the gallbladder. If bile builds up within your gallbladder, causing cholecystitis, the bile may become infected.
- Death of gallbladder tissue. Untreated cholecystitis can cause tissue in the gallbladder to die (gangrene). It's the most common complication, especially among older people, those who wait to get treatment and those with diabetes. This can lead to a tear in the gallbladder, or it may cause your gallbladder to burst.
- Torn gallbladder. A tear (perforation) in your gallbladder may result from gallbladder swelling, infection or death of tissue.
Prevention
You can reduce your risk of cholecystitis by taking the following steps to prevent gallstones:
- Lose weight slowly. Rapid weight loss can increase the risk of gallstones.
- Maintain a healthy weight. Being overweight makes you more likely to develop gallstones. To achieve a healthy weight, reduce calories and increase your physical activity. Maintain a healthy weight by continuing to eat well and exercise.
- Choose a healthy diet. Diets high in fat and low in fiber may increase the risk of gallstones. To lower your risk, choose a diet high in fruits, vegetables and whole grains.
Diagnosis
To diagnose cholecystis, your health care provider will likely do a physical exam and discuss your symptoms and medical history. Tests and procedures used to diagnose cholecystitis include:
- Blood tests. Your health care provider may order blood tests to look for signs of an infection or signs of gallbladder problems.
- Imaging tests that show your gallbladder. Abdominal ultrasound, endoscopic ultrasound, computerized tomography (CT) scan or magnetic resonance cholangiopancreatography (MRCP) can be used to create pictures of your gallbladder and bile ducts. These pictures may show signs of cholecystitis or stones in the bile ducts and gallbladder.
- A scan that shows the movement of bile through your body. A hepatobiliary iminodiacetic acid (HIDA) scan tracks the production and flow of bile from your liver to your small intestine. A HIDA scan involves injecting a radioactive dye into your body, which attaches to bile-producing cells. During the scan, the dye can be seen as it travels with the bile through the bile ducts. This can show any blockages.
Treatment
Treatment for cholecystitis usually involves a hospital stay to control the inflammation in your gallbladder. Sometimes, surgery is needed.
At the hospital, your health care provider will work to control your symptoms. Treatments may include:
- Fasting. You may not be allowed to eat or drink at first in order to take stress off your inflamed gallbladder.
- Fluids through a vein in your arm. This treatment helps prevent dehydration.
- Antibiotics to fight infection. If your gallbladder is infected, your provider likely will recommend antibiotics.
- Pain medications. These can help control pain until the inflammation in your gallbladder is relieved.
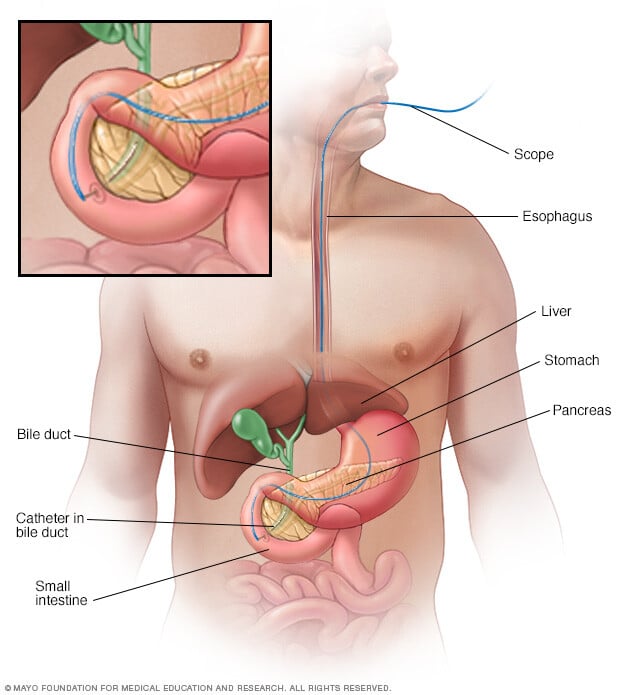
- Procedure to remove stones. You may have a procedure called an endoscopic retrograde cholangiopancreatography (ERCP). During this procedure that uses dye to highlight the bile ducts, instruments can be used to remove stones blocking the bile ducts or cystic duct.
- Gallbladder drainage. In some cases, such as when surgery to remove the gallbladder is not an option, gallbladder drainage (cholecystostomy) may be done to remove infection. Drainage is done through the skin on the abdomen (percutaneous) or by passing a scope through the mouth (endoscopic).
Your symptoms are likely to decrease in 2 to 3 days. However, gallbladder inflammation often returns. Most people with cholecystitis eventually need surgery to remove the gallbladder.
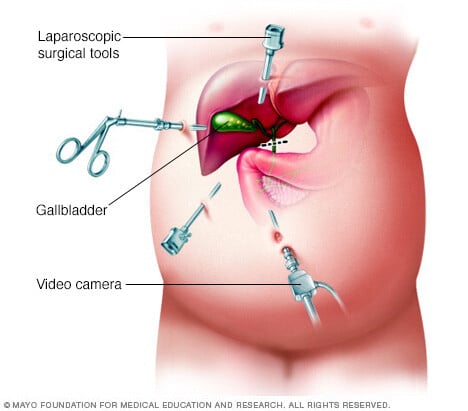
Gallbladder removal surgery
The procedure to remove the gallbladder is called a cholecystectomy. Usually, this is a minimally invasive procedure, involving a few tiny cuts (incisions) in your abdomen (laparoscopic cholecystectomy). An open procedure, in which a long incision is made in your abdomen, is rarely required.
The timing of surgery depends on the severity of your symptoms and your overall risk of problems during and after surgery. If you're at low surgical risk, surgery may be performed during your hospital stay.
Once your gallbladder is removed, bile flows directly from your liver into your small intestine, rather than being stored in your gallbladder. Even without your gallbladder you can still digest food.
Preparing for an appointment
Make an appointment with your health care provider if you have symptoms that worry you. If your provider suspects that you have cholecystitis, you may be referred either to a specialist in the digestive system (gastroenterologist) or you may be sent to a hospital.
What you can do
Before your appointment:
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet.
- Make a list of your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Make a list of key personal information, including major stresses or recent life changes.
- Make a list of all medications, vitamins, herbs and other supplements that you're taking.
- Take a family member or friend along, if possible. Someone who accompanies you can help you remember the information you get.
- Make a list of questions to ask your health care provider.
For cholecystitis, some basic questions to ask include:
- Is cholecystitis the likely cause of my abdominal pain?
- What are other possible causes for my symptoms?
- What tests do I need?
- Do I need gallbladder removal surgery?
- How soon do I need surgery?
- What are the risks of surgery?
- How long does it take to recover from gallbladder surgery?
- Are there other treatment options for cholecystitis?
- Should I see a specialist?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
Don't hesitate to ask other questions, as well.
What to expect from your doctor
Your health care provider is likely to ask you a number of questions, including:
- When did your symptoms begin?
- Have you had pain like this before?
- Are your symptoms constant or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?



