Cavernous malformations
Overview
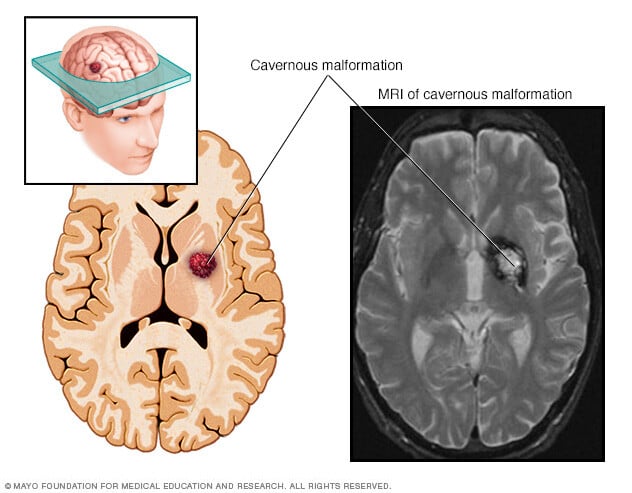
Cerebral cavernous malformations (CCMs) are groups of tightly packed, irregular small blood vessels with thin walls. They may be present in the brain or spinal cord. The vessels contain slow-moving blood that's usually clotted. CCMs look like small mulberries. In some people, CCMs can cause blood to leak in the brain or spinal cord.
CCMs vary in size. Often they are less than half an inch (1 centimeter). Most CCMs are sporadic. This means the CCM occurs as a single cavernous malformation and there isn't a family history. But about 20% of CCMs affect people of the same family. These are known as familial CCMs. Familial CCMs are related to a gene change passed down through families. People with familial CCMs usually have multiple cavernous malformations.
A CCM is one of several types of brain vascular malformations that contain irregular blood vessels. Other types of vascular malformations include:
- Arteriovenous malformation (AVM).
- Dural arteriovenous fistula.
- Developmental venous anomaly (DVA).
- Capillary telangiectasia.
For people who have the sporadic form, it's common to have both a DVA and a CCM.
CCMs may leak blood and lead to bleeding in the brain or spinal cord, known as a hemorrhage. Brain hemorrhages can cause many symptoms, such as seizures.
Depending on the location, CCMs also can cause stroke-like symptoms such as trouble with movement or feeling in the legs and sometimes the arms. CCMs also may cause bowel and bladder symptoms.
Symptoms
Cerebral cavernous malformations (CCMs) may not cause symptoms. Sometimes when the CCM occurs on the outer surface of the brain, it can cause seizures.
And CCMs found in other areas can have a variety of symptoms. These include CCMs in the spinal cord, the brainstem linking the spinal cord and brain, and the basal ganglia in the inner brain. For example, bleeding in the spinal cord may cause bowel and bladder symptoms or trouble with movement or feeling in the legs or arms.
Generally, symptoms of CCMs may include:
- Seizures.
- Bad headaches.
- Weakness in the arms or legs.
- Numbness.
- Trouble speaking.
- Poor memory and attention.
- Trouble balancing and walking.
- Vision changes, such as double vision.
Symptoms can get worse over time with repeated bleeding. Bleeding can happen again soon after the first bleed or much later. In some people, a repeat bleed may never occur.
When to see a doctor
Seek medical help right away if you experience any symptoms of a seizure. Also get immediate medical help if you have symptoms that suggest a cerebral cavernous malformation or brain bleeding.
Causes
Most cerebral cavernous malformations (CCMs) are known as the "sporadic form." They occur as a single malformation without any family history. The sporadic form often has an associated developmental venous anomaly (DVA), which is an irregular vein with a witch's broom appearance.
However, about 20% of people with a CCM have a genetic form. This form is passed down in families, known as familial cavernous malformation syndrome. People with this form may have family members with CCMs, most often with more than one malformation. A diagnosis can be confirmed by a genetic test that requires a blood or saliva sample. Genetic testing is often recommended for people who have:
- MRI evidence of multiple CCMs without a DVA.
- A family history of CCMs.
Radiation to the brain or spinal cord also may result in CCMs within 2 to 20 years afterward. Other rare syndromes may be associated with CCM.
Risk factors
Most cerebral cavernous malformations (CCMs) have no clear cause. But the form that's passed down through families can cause multiple CCMs, both to start with and over time.
To date, research has identified three genetic changes responsible for cavernous malformations passed down through families. Almost all familial cases of cavernous malformations have been traced through those genetic changes.
Familial CCMs are passed down in families through a change in one of these genes:
- KRIT1, also called CCM1.
- CCM2.
- PDCD10, also called CCM3.
These genes are responsible for affecting the leakiness of blood vessels and the proteins that keep the blood vessel cells together.
Complications
The most serious complications of cerebral cavernous malformations (CCMs) stem from repeated bleeding, known as hemorrhages. CCMs that bleed over and over again may cause a hemorrhagic stroke and lead to damage in the nervous system.
Bleeding is more likely to return in people with prior hemorrhages. Bleeding also is more likely to happen again with CCMs located in the brainstem.
Diagnosis

Often people with cerebral cavernous malformations (CCMs) don't have any symptoms. A CCM may be found as a result of brain imaging for another condition. Sometimes specific symptoms may prompt your healthcare professional to do more testing.
Tests
Depending on why the condition is suspected, your healthcare professional may order tests to confirm CCMs or to identify or rule out other related conditions. You may have imaging tests to look for changes in the blood vessels. Your healthcare professional also may order tests if you have already been diagnosed with a CCM and have new symptoms. The tests can show if there's bleeding or new CCMs.
- Magnetic resonance imaging (MRI). In this test, a detailed picture is made of your brain or spine. Sometimes a contrast dye is injected into a vein in the arm.
- Genetic testing. If you have a family history of the condition, genetic counseling and blood or saliva tests can help find gene changes related with CCMs.
Treatment

Cerebral cavernous malformations (CCMs) are treated by specialists. They may include:
- Doctors trained in brain and nervous system conditions, known as neurologists and cerebrovascular neurologists.
- Doctors trained in brain and nervous system surgery, known as neurosurgeons.
- Doctors trained in brain imaging, known as neuroradiologists.
Doctors trained in other specialties also may be involved in your treatment.
Your healthcare team reviews your symptoms and imaging tests to decide on a treatment plan. The care team may recommend closely watching the cavernous malformation is recommended. Or your care team may recommend removing or treating the cavernous malformation. Several options exist for treating a cavernous malformation surgically. And research is looking into medicines that can reduce bleeding risk.
If you have seizures related to a cavernous malformation, you may be prescribed medicines to stop the seizures.
Potential future treatments
Experts are looking at using imaging technology to improve predictions of the course of disease in some people. They're also looking at using imaging to get more information about a particular individual's disease state. These technologies include imaging through quantitative susceptibility mapping and permeability imaging using dynamic contrast-enhanced MRI.
Several medicines are being tested in clinical trials to see if specific medicines — rather than surgery — could reduce the chance of further bleeding. Talk to your healthcare professional about which clinical trials may be available to you.
Preparing for an appointment
See your healthcare professional if you have any symptoms that worry you. If a cerebral cavernous malformation is suspected, a referral to an experienced specialist can provide the best outcome.
Here's some information to help you get ready for the appointment, and what to expect from your healthcare professional.
What you can do
- Keep a detailed symptoms calendar. Each time a symptom occurs, write down the time, what you experienced and how long it lasted.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking.
- Take a family member or friend along. Sometimes it can be hard to remember all the information provided to you during an appointment. Someone who comes with you may remember something that you missed or forgot.
- Bring any recent brain scans in a CD to your appointment.
Also, if you've experienced seizures, your healthcare professional may want to ask questions of someone who has witnessed them. It's common not to be aware of everything that happens when you experience a seizure.
Write down questions to ask your healthcare professional
Prepare a list of questions to help you make the most of your time. List your questions from most important to least important. Here are some examples of questions to ask.
General questions
- How many cavernous malformations do I have?
- Where is it, or where are they located?
- What functions do the area or areas of the brain perform?
- Should I have genetic tests?
- Should my children or anyone else in my family be tested?
Management and observation
- How often will I need follow-up tests?
- How often will I follow up with you?
Surgery to remove a malformation
- How long would you estimate I'd be in surgery?
- How long does surgery recovery usually take?
- How long should I plan to be in the hospital?
Surgical background
- How many CCMs have you seen, and how many have you treated?
- Does your institution have a cerebrovascular specialty practice?
Other questions may be useful for your needs. The Alliance to Cure Cavernous Malformation offers lists of suggested questions.
Don't hesitate to ask any other questions during your appointment if you don't understand something.
What to expect from your doctor
You're likely to be asked a number of questions:
- When did you first begin experiencing symptoms? For example, when did headaches, seizures, bleeding, or weakness in your arms or legs start? When did you begin to have trouble with vision, balance, speech, memory or attention?
- Do your symptoms come and go, or are they present all the time?
- Do your symptoms seem to be triggered by certain events or conditions?
What you can do in the meantime
Certain conditions and activities can trigger seizures, so it may be helpful to:
- Not drink too much alcohol.
- Not use nicotine.
- Get enough sleep.
- Reduce stress.



