Polycystic kidney disease
Overview
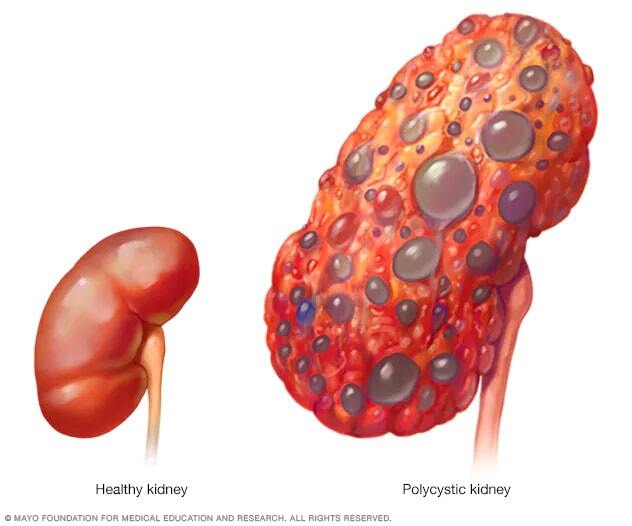
Polycystic kidney disease (PKD) is a condition in which clusters of cysts grow in the body, mainly in the kidneys. Over time, the cysts may cause the kidneys to get bigger and stop working. PKD is most often passed through families. This is called an inherited condition.
Cysts are round sacs with fluid in them. They are not cancer. In PKD, the cysts vary in size. They can grow very large. Having many cysts or large cysts can damage the kidneys.
Polycystic kidney disease also can cause cysts to grow in the liver, the pancreas and other places in the body. The disease can cause serious complications, including high blood pressure and kidney failure.
PKD varies greatly in how bad it is. It's possible to prevent some complications. Lifestyle changes and treatments might help reduce damage to the kidneys.
Symptoms
Polycystic kidney disease symptoms can include:
- High blood pressure.
- Belly, side or back pain.
- Blood in the urine.
- A feeling of fullness in the belly.
- Increased size of the belly from enlarged kidneys.
- Headaches.
- Kidney stones.
- Kidney failure.
- Urinary tract or kidney infections.
When to see a doctor
People often have polycystic kidney disease for years without knowing it.
If you have some of the symptoms of polycystic kidney disease, see your healthcare professional. If you have a parent, sibling or child with polycystic kidney disease, see your healthcare professional to talk about screening for the condition.
Causes
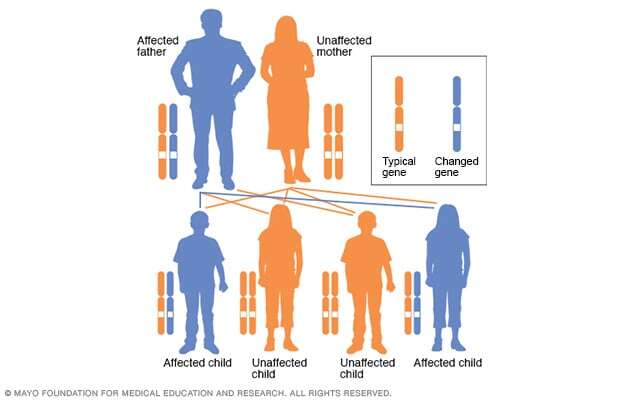

Gene changes cause polycystic kidney disease. Most often, the condition runs in families. Sometimes, a gene change happens on its own in a child. This is known as a spontaneous gene change. Then neither parent has a copy of the changed gene.
There are two main types of polycystic kidney disease. They're caused by different gene changes. The two types of PKD are:
-
Autosomal dominant polycystic kidney disease (ADPKD). This is the most common type of ongoing kidney disease that's passed through families, also called inherited. Symptoms of ADPKD often start between the ages of 30 and 40.
Only one parent needs to have the condition to pass it to the children. If one parent has ADPKD, each child has a 50% chance of getting the condition. This is the more common type of polycystic kidney disease.
-
Autosomal recessive polycystic kidney disease (ARPKD). This type is far less common than is ADPKD. The symptoms often appear soon after birth. Sometimes, symptoms don't appear until later in childhood or during the teen years.
Both parents must have gene changes to pass on this form of the condition. If both parents carry a changed gene, each child has a 25% chance of getting the condition.
Risk factors
The biggest risk factor for getting polycystic kidney disease is getting the gene changes that cause the disease from one or both parents.
Complications
Complications linked to polycystic kidney disease include:
- High blood pressure. This is common in polycystic kidney disease. Not treated, high blood pressure can cause more damage to the kidneys and increase the risk of heart disease and strokes.
- Loss of kidney function. The kidneys' losing their ability to do their work is one of the most serious complications of polycystic kidney disease. Nearly half of people with the condition have kidney failure by age 60. But for some people, it starts in the early 30s.
- Pain. It's common to have pain with polycystic kidney disease. Pain often is in the side or back. The pain can come and go or be ongoing. The pain may be linked to bleeding into a cyst, a urinary tract infection, a kidney stone or, less often, cancer.
-
Cysts in the liver. The older people with polycystic kidney disease get, the more likely it is they'll get cysts in the liver. With cysts, the liver most often keeps working.
Women tend to get larger cysts than do men. Hormones and pregnancies might be part of the reason.
-
Brain aneurysm. A balloonlike bulge in a blood vessel, called an aneurysm, in the brain can cause bleeding if it bursts. People with polycystic kidney disease have a higher risk of aneurysms. People with a family history of aneurysms seem to be at highest risk.
Ask your healthcare professional if you need screening. If screening doesn't show an aneurysm, your healthcare professional may suggest screening again in a few years. The timing of repeat screening depends on your risk.
- Pregnancy complications. Most people with polycystic kidney disease can have success with pregnancy. But sometimes, they can get a life-threatening condition called preeclampsia during pregnancy. Those most at risk have high blood pressure or a loss of kidney function before they become pregnant.
- Heart valve conditions. As many as 1 in 4 adults with polycystic kidney disease gets mitral valve prolapse. When this happens, the heart valve no longer closes well. This lets blood leak backward.
- Colon conditions. People with polycystic kidney disease may get weaknesses and pouches or sacs called diverticula in the wall of the colon. This condition is called diverticulosis. Diverticula most often don't cause symptoms, but they may bleed or get infected.
Prevention
If you have polycystic kidney disease and you're thinking about having children, a genetic counselor can help you know your risk of passing the disease to your children.
Keeping your kidneys as healthy as possible may help prevent some of the complications of this disease. It's most important to manage your blood pressure.
Here are some tips for keeping your blood pressure in check:
- Take the blood pressure medicines your healthcare professional prescribes as directed.
- Eat a low-salt diet that has plenty of fruits, vegetables and whole grains.
- Get to and stay at a healthy weight.
- Exercise regularly. Aim for at least 30 minutes of moderate physical activity most days of the week.
- Limit alcohol use.
- Don't smoke.
Diagnosis
For polycystic kidney disease, certain tests can detect the size and number of kidney cysts you have. Tests also can show how much healthy kidney tissue you have. Tests include:
- MRI scan. As you lie inside a large cylinder, magnetic fields and radio waves show views of your kidneys. This method most often is used to know how badly PKD affects the kidneys, liver or pancreas. MRI can help measure total kidney volume, which helps healthcare professionals know more about your condition.
- Ultrasound. This involves putting a wandlike device called a transducer on your body. It gives off sound waves that go back to the transducer. A computer turns the sound waves into images of your kidneys.
- CT scan. You lie on a table that goes into a big, doughnut-shaped device. The device uses X-ray beams to show images of your kidneys.
Treatment
How bad polycystic kidney disease is varies from person to person. That's true even among people in the same family. Often, people with PKD reach end-stage kidney disease between ages 55 and 65. But some people with PKD have mild disease. They might never get to end-stage kidney disease.
Treating polycystic kidney disease involves dealing with the following symptoms and complications in their early stages:
-
Kidney cyst growth. The medicine tolvaptan (Jynarque, Samsca) may be used for adults at risk of ADPKD that's getting worse fast. Tolvaptan is a pill that you swallow that slows how fast kidney cysts grow. It also slows the decline in how well your kidneys work.
Tolvaptan carries a risk of serious liver injury. And it can interact with other medicines you take. It's best to see a specialist in kidney health, called a nephrologist. A nephrologist can watch for side effects and possible complications of the medicine.
-
High blood pressure. Keeping high blood pressure under control can slow the disease and kidney damage. Eating a low-sodium, low-fat diet that's moderate in protein and calories and drinking more fluids may help control blood pressure.
Other helpful lifestyle changes include not smoking, moving more and easing stress. Smoking can greatly harm the kidneys. It also can speed up the start of kidney failure.
Medicines most often are needed to control high blood pressure. Medicines called angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are often used to control high blood pressure.
- Loss of kidney function. To help your kidneys stay as healthy as possible for as long as possible, experts suggest being at a healthy weight and body mass index. Drinking water and fluids throughout the day may help slow the growth of kidney cysts. This could slow the loss of kidney function. Eating a low-salt diet with less protein might let kidney cysts respond better to more fluids.
-
Pain. You might be able to control the pain of polycystic kidney disease with medicines available without a prescription, such as acetaminophen (Tylenol, others). Don't take nonsteroidal anti-inflammatory medicines such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve). Long-term use of nonsteroidal anti-inflammatory medicines can affect how your kidneys work.
For worse pain, a healthcare professional might use a needle to draw out cyst fluid and put in a medicine to shrink kidney cysts. The medicine is called a sclerosing agent.
Or you may need surgery to remove cysts if they're large enough to cause pressure and pain. The surgery is called cyst fenestration.
- Bladder or kidney infections. Treating infections quickly with antibiotics can help prevent kidney damage. You might have a simple bladder infection or a more complicated cyst or kidney infection. For more-complicated infections, you may need to take antibiotics longer.
-
Blood in the urine. Drink lots of fluids as soon as you notice blood in your urine. It's best to drink water to dilute the urine. This might help prevent clots from forming in your urinary tract.
Most often, the bleeding stops on its own. If it doesn't, call your healthcare professional.
-
Kidney failure. Your kidneys can stop removing waste and extra fluids from your blood. Then you need either dialysis or a kidney transplant. That's why you need to see your healthcare team regularly.
You may be able to have a kidney transplant before your kidneys fail. Then you wouldn't need to have dialysis. This is called preemptive kidney transplantation.
-
Aneurysms. If you have polycystic kidney disease and a family history of brain aneurysms that burst, your healthcare team may want to do regular screenings for brain aneurysms.
If you have an aneurysm, surgical clipping might reduce the risk of bleeding. This depends on the size of the aneurysm. Nonsurgical treatment of small aneurysms may involve controlling high blood pressure and high blood cholesterol, as well as quitting smoking.
Early treatment offers the best chance of slowing the progress of polycystic kidney disease.
Coping and support
Having polycystic kidney disease might feel hard to bear. The support of friends and family can help you deal with having the condition. Also, talking with a counselor, psychologist, psychiatrist or clergy member may help.
You also might join a support group. For some people, support groups can have helpful information about treatments and coping. And being with people who know what you're going through might make you feel less alone.
Ask your healthcare team about support groups in your area.
Preparing for an appointment
You're likely to start by seeing your primary health professional. Then you might be referred to a specialist in kidney health, called a nephrologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before certain tests. Make a list of:
- Your symptoms, including any that don't seem linked to the reason for your appointment, and when they began.
- All medicines, vitamins and other supplements you take, including dosages.
- Your and your family's medical history. Be sure to include any history of kidney conditions.
- Questions to ask your care team.
Take a family member or friend with you if you can. Someone who goes with you can help you remember the information you get.
For polycystic kidney disease, questions to ask include:
- What's the most likely cause of my symptoms?
- Are there other possible causes for my symptoms?
- What tests do I need?
- How bad is my condition? Do you have an idea of when I will reach kidney failure or need a kidney transplant or dialysis?
- Is this condition likely to go away or last long?
- What's the best course of action?
- What can be done to keep my cystic disease from getting worse?
- I have other health conditions. How can I best manage them together?
- Do I need to restrict my diet or activities?
- Are there brochures or other printed material that I can have? What websites do you suggest?
Be sure to ask all the questions you have.
What to expect from your doctor
Your care team is likely to ask you questions, such as:
- Do you always have symptoms or do they come and go?
- Does anything seem to make your symptoms better or worse?
- Do you know what your blood pressure typically is?
- Has your kidney function been measured?



