Pericarditis
Overview
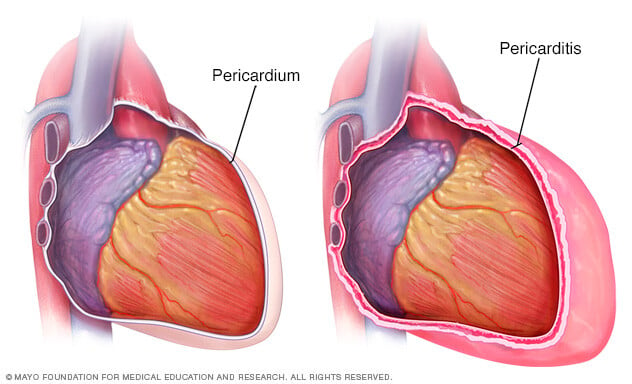
Pericarditis is swelling and irritation of the thin, saclike tissue surrounding the heart. This tissue is called the pericardium. Pericarditis often causes sharp chest pain. The chest pain occurs when the irritated layers of the pericardium rub against each other.
Pericarditis often is mild. It may go away without treatment. Treatment for more-serious symptoms can include medicines and, very rarely, surgery. When healthcare professionals find and treat pericarditis early, that may help lower the risk of long-term complications from pericarditis.
Symptoms
Chest pain is the most common symptom of pericarditis. It usually feels sharp or stabbing. But some people have dull, achy or pressure-like chest pain.
Most often, pericarditis pain is felt behind the breastbone or on the left side of the chest. The pain may:
- Spread to the left shoulder and neck, or to both shoulders.
- Get worse when coughing, lying down or taking a deep breath.
- Get better when sitting up or leaning forward.
Other symptoms of pericarditis can include:
- Cough.
- Fatigue or general feeling of weakness or being sick.
- Swelling of the legs or feet.
- Low-grade fever.
- Pounding or racing heartbeat, also called heart palpitations.
- Shortness of breath when lying down.
- Swelling of the belly, also called the abdomen.
The specific symptoms depend on the type of pericarditis. Pericarditis is grouped into different categories, according to the pattern of symptoms and how long symptoms last.
- Acute pericarditis begins suddenly but doesn't last longer than four weeks. Future episodes can occur. It may be hard to tell the difference between acute pericarditis and pain due to a heart attack.
- Recurrent pericarditis occurs about 4 to 6 weeks after a bout of acute pericarditis. No symptoms happen in between.
- Incessant pericarditis lasts about 4 to 6 weeks but less than three months. The symptoms continue over this whole time.
- Chronic constrictive pericarditis usually develops slowly and lasts longer than three months.
When to see a doctor
Get medical care right away if you have new symptoms of chest pain.
Many of the symptoms of pericarditis are like those of other heart and lung conditions. It's important to be thoroughly checked by a healthcare professional if you have any type of chest pain.
Causes
The cause of pericarditis is often hard to determine. A cause may not be found. When this happens, it's called idiopathic pericarditis.
Pericarditis causes can include:
- Immune system response after heart damage due to a heart attack or heart surgery. Other names for this include Dressler syndrome, post-myocardial infarction syndrome and post-cardiac injury syndrome.
- Infections, such as those caused by viruses.
- Injury to the heart or chest.
- Lupus.
- Rheumatoid arthritis.
- Other long-term health conditions, including kidney failure and cancer.
- Some medicines, such as the seizure treatment phenytoin (Dilantin) and medicine called procainamide to treat an irregular heartbeat.
Complications
When pericarditis is found and treated early, the risk of complications usually becomes lower. Complications of pericarditis can include:
- Fluid buildup around the heart, also called pericardial effusion. The fluid buildup can lead to further heart complications.
- Thickening and scarring of the heart lining, also called constrictive pericarditis. Some people with long-term pericarditis develop permanent thickening and scarring of the pericardium. The changes prevent the heart from filling and emptying properly. This complication often leads to severe swelling of the legs and abdomen, and shortness of breath.
- Pressure on the heart due to fluid buildup, also called cardiac tamponade. This life-threatening condition prevents the heart from filling properly. Less blood leaves the heart, causing a large drop in blood pressure. Cardiac tamponade requires emergency treatment.
Prevention
There's no specific way to prevent pericarditis. But you can take these steps to prevent infections, which might help lower the risk of heart inflammation:
- Stay away from people who have a viral or flu-like illness until they've recovered. If you're sick with symptoms of a viral infection, try not to expose others. For instance, cover your mouth when you sneeze or cough.
- Follow good hygiene. Regular hand-washing can help prevent spreading illness. Scrub your hands with soap and water for at least 20 seconds.
- Get recommended vaccines. Stay up to date on the recommended vaccines, including those that protect against COVID-19, rubella and influenza. These are examples of viral diseases that can cause inflammation of the heart muscle, called myocarditis. Myocarditis and pericarditis can happen together due to a viral infection. Rarely, the COVID-19 vaccine can cause pericarditis and myocarditis, especially in males ages 12 through 17. Talk to your healthcare professional about the benefits and risks of vaccines.
Diagnosis
To diagnose pericarditis, a healthcare professional examines you and asks questions about your symptoms and medical history.
The care professional listens to your heart using a device called a stethoscope. Pericarditis causes a specific sound, called a pericardial rub. The noise occurs when the two layers of the sac surrounding the heart, called the pericardium, rub against each other.
Tests
Tests to diagnose pericarditis or rule out conditions that may cause similar symptoms may include:
- Blood tests. Blood tests usually are done to check for signs of a heart attack, inflammation and infection.
- Electrocardiogram (ECG). An electrocardiogram is a quick and painless test that records the electrical signals in the heart. It can show how the heart is beating. Sticky patches called electrodes with wires attach to the chest and sometimes the arms or legs. The wires connect to a monitor, which prints or displays results.
- Chest X-ray. A chest X-ray can show changes in the size and shape of the heart. It can tell if the heart is enlarged.
- Echocardiogram. Sound waves create images of the moving heart. An echocardiogram shows how well the heart is pumping blood. It also can see any fluid buildup in the tissue surrounding the heart. The test can tell if the sac surrounding the heart affects the way the heart fills with blood or pumps blood.
- Cardiac computerized tomography (CT) scan. Cardiac CT scans use X-rays to create images of the heart and chest. The test can be used to look for heart thickening that may be a sign of constrictive pericarditis.
- Cardiac magnetic resonance imaging (MRI). This test uses magnetic fields and radio waves to create detailed images of the heart. A cardiac MRI scan can show thickening, inflammation or other changes in the thin tissue surrounding the heart.
Treatment
Treatment for pericarditis depends on the cause of the symptoms and how serious they are. Mild pericarditis may get better without treatment.
Medications
Medicines often are used to treat symptoms of pericarditis. Examples include:
- Pain relievers. Pericarditis pain often can be treated using pain relievers sold without a prescription. These include aspirin and ibuprofen (Advil, Motrin IB, others). Talk with your healthcare professional before you take any non-prescription medicine. Take any medicine as directed. Sometimes, prescription-strength pain relievers are used to ease pericarditis pain.
- Colchicine (Colcrys, Mitigare, others). This medicine lowers inflammation in the body. It's used to treat sudden pericarditis or if symptoms tend to come back. You should not take colchicine if you have liver or kidney disease. Colchicine also can affect other medicines. Your healthcare professional checks your health history before prescribing colchicine.
- Corticosteroids. Corticosteroids are strong medicines that fight inflammation. A corticosteroid such as prednisone may be given if pericarditis symptoms don't get better with other medicines. Corticosteroids also might be prescribed if symptoms keep coming back.
- Immunosuppressants. These medicines turn down the immune system to lower the inflammation it makes. They may be used when a condition such as rheumatoid arthritis causes pericarditis.
- Immunomodulators. These medicines change the immune system's activity to help control inflammation. One type of immunomodulator that can be used to treat pericarditis is called an interleukin 1 blocker.
If pericarditis is caused by a bacterial infection, treatment may include antibiotics. Extra fluid in the space between the pericardium's layers also may need to be drained.
Surgeries or other procedures
If pericarditis causes fluid buildup around the heart, a surgery or other procedure may be needed to drain the fluid.
Surgeries or other procedures to treat pericarditis include:
- Pericardiocentesis. In this procedure, a sterile needle or a small tube called a catheter is used to remove and drain the excess fluid from the pericardium.
- Removal of the pericardium, also called pericardiectomy. Part or all of the pericardium may need to be removed. This is done if the sac surrounding the heart stays rigid due to constrictive pericarditis.
Lifestyle and home remedies
Lifestyle and home remedies for mild pericarditis include rest and pain medicines sold without a prescription. If your healthcare professional recommends pain medicines, take them as directed.
While you recover, do not take part in strenuous physical activity and competitive sports. Such activity can trigger pericarditis symptoms. Ask your healthcare professional how long you need to rest.
Preparing for an appointment
You're likely to start by seeing a primary care professional or an emergency room doctor. You may be referred to a doctor trained in heart diseases. This type of care professional is called a cardiologist.
Here's some information to help you prepare for your appointment.
What you can do
When you make your appointment, ask if you need to do anything in advance, such as avoid food or drinks.
Write down the following information and take it with you to the appointment:
- Write down any symptoms you're having and for how long you've had them. Also note if you've had similar symptoms that have come and gone in the past.
- Make a list of important medical information. Include other recent health concerns you've had.
- Write down the names of any medicines you take. Include the dosages.
- Ask someone to come with you to the appointment, if possible. Someone who goes with you can help remember what the healthcare professional says.
- Write down the questions you want to be sure to ask your healthcare team.
For pericarditis, some basic questions to ask your healthcare professional include:
- What's the most likely cause of my symptoms?
- What kinds of tests do I need? Will I need to stay in the hospital for testing?
- What treatment approach do you recommend?
- How soon after I begin treatment can I expect my symptoms to get better?
- What are the possible side effects of the treatments you're prescribing?
- Am I at risk of long-term complications from this condition?
- How often will I need follow-up appointments for this condition?
- Do I need to follow any activity or diet restrictions?
- Are there any special guidelines for managing this condition along with my other health conditions?
Feel free to ask other questions that occur to you during your appointment.
What to expect from your doctor
Your healthcare team usually asks you some questions. Being ready to answer them may save time to go over any details you want to talk about in-depth. Your healthcare team may ask:
- Can you describe your symptoms? Where is the pain? How severe is the pain?
- When did your symptoms start?
- Did your symptoms come on slowly or suddenly?
- Have you had similar symptoms in the past?
- Are you having any trouble breathing?
- Does changing your position affect your pain?
- Have you recently had a cold or the flu? What about a fever?
- Have you recently lost weight without trying?
- Do you have a parent, brother, sister or child with a history of heart disease?
- Do you or did you smoke? How much?



