Post-polio syndrome
Overview
Post-polio syndrome is a group of potentially disabling signs and symptoms that appear decades after the initial polio illness. These signs and symptoms usually appear between 30 to 40 years after having polio.
Infection from the polio virus once caused paralysis and death. However, the introduction of the inactivated polio vaccine in the 1950s greatly reduced polio's spread.
Today, very few people in developed countries are paralyzed from the polio virus, usually related to a reaction from one form of the vaccine. However, there remain many people who had polio at a young age who now later in life might develop the post-polio syndrome.
Symptoms
Post-polio syndrome only affects people who had polio. Common signs and symptoms of post-polio syndrome include:
- Muscle and joint weakness and pain that gets worse over time
- Feeling easily fatigued and exhausted
- Losing muscle tissue (atrophy)
- Breathing or swallowing problems
- Sleep-related breathing disorders, such as sleep apnea
- Decreased tolerance of cold temperatures
Post-polio syndrome progresses slowly in most people. They may experience new signs and symptoms followed by periods of stability.
When to see a doctor
See your doctor if you have increasing weakness or fatigue. It's important to rule out other causes of your signs and symptoms and determine whether you have post-polio syndrome.
Causes
There are several theories as to what causes post-polio syndrome, but no one knows for sure.
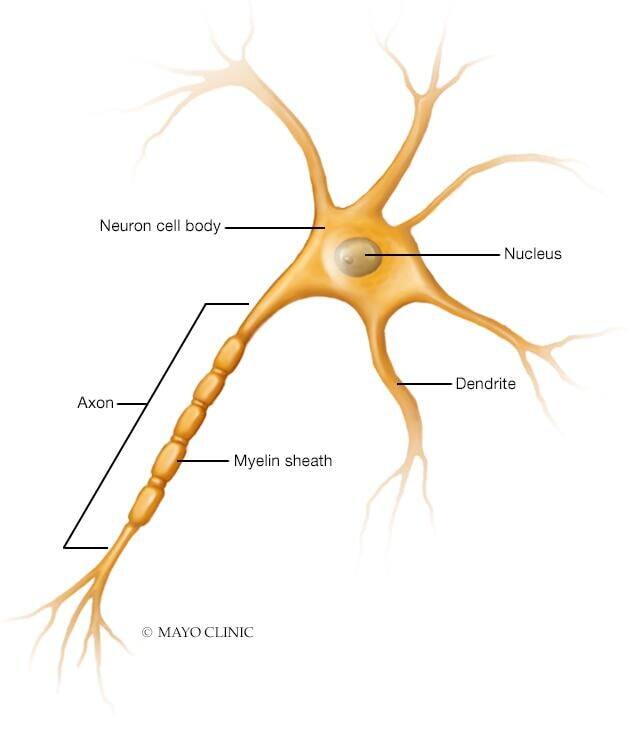
When poliovirus infects your body, it affects nerve cells called motor neurons that carry messages (electrical impulses) between your brain and your muscles. Poliovirus particularly affects the motor neurons in the spinal cord.
Each motor neuron consists of three basic components:
- A cell body
- A major branching fiber (axon)
- Numerous smaller branching fibers (dendrites)
A polio infection often damages or destroys many of these motor neurons. Because there are fewer motor neurons, the remaining neurons sprout new fibers and grow bigger.
This promotes recovery of the use of your muscles, but it also may stress the nerve cell body to nourish the additional fibers. Over the years, this stress may be too much. This may cause the gradual breakdown of the sprouted fibers and, eventually, of the neuron itself.
Risk factors
Factors that can increase your risk of developing post-polio syndrome include:
- Severity of initial polio infection. The more severe the initial infection, the more likely that you'll have signs and symptoms of post-polio syndrome.
- Age at onset of initial illness. If you developed polio as an adolescent or adult rather than as a child, your chances of developing post-polio syndrome increase.
- Recovery. The greater your recovery after acute polio, the more likely it seems that post-polio syndrome will develop. This may be because greater recovery places additional stress on motor neurons.
- Excessive physical activity. If you often exercise to the point of exhaustion or fatigue, you might overwork already stressed-out motor neurons and increase your risk of post-polio syndrome.
Complications
Post-polio syndrome is rarely life-threatening, but severe muscle weakness can lead to complications:
- Falls. Weakness in your leg muscles makes it easier for you to lose your balance and fall. You then might break a bone, such as a hip, leading to other complications.
- Fatigue. Fatigue is very common in people with post-polio syndrome. The fatigue may be disabling, even after very little activity. It may also lead to problems with concentration and memory.
- Pain. Musculoskeletal abnormalities and muscle weakness can lead to chronic pain.
-
Malnutrition, dehydration and pneumonia. People who've had bulbar polio, which affects nerves leading to muscles involved in chewing and swallowing, often have difficulty with these activities and have other signs of post-polio syndrome.
Chewing and swallowing problems can lead to inadequate nutrition and to dehydration, as well as to aspiration pneumonia, which is caused by inhaling food particles into your lungs (aspirating).
-
Chronic respiratory failure. Weakness in your diaphragm and chest muscles makes it harder to take deep breaths and cough, which can cause fluid and mucus to build up in your lungs.
Obesity, smoking, curvature of the spine, anesthesia, prolonged immobility and certain medications can further decrease your breathing ability, possibly leading to a sharp drop in blood oxygen levels (acute respiratory failure). You might then need treatment to help you breathe (ventilation therapy).
- Osteoporosis. Prolonged inactivity and immobility are often accompanied by loss of bone density and osteoporosis in both men and women. If you have post-polio syndrome, talk to your doctor about bone density screening.
- Sleep disorders. Sleep apnea and restless legs syndrome are common in people with post-polio syndrome. These sleep disorders may worsen insomnia and fatigue if untreated.
Diagnosis
There's no specific test to diagnose post-polio syndrome. Diagnosis is based on a medical history and physical exam, and exclusion of other conditions that could cause the signs and symptoms.
Indicators of post-polio syndrome
For a diagnosis of post-polio syndrome, doctors look for three indicators:
- Previous diagnosis of polio. This might require finding old medical records or getting information from older family members.
- Long interval after recovery. People who recover from the initial attack of polio often live for years without further signs or symptoms. The onset of late effects varies widely but typically begins at least 15 years after the initial diagnosis.
- Gradual onset. The later onset weakness typically occurs in muscles that were affected at the time of the initial polio illness. Weakness often isn't noticeable until it interferes with daily activities. You might awaken refreshed but feel exhausted by the early afternoon, tiring after activities that were once easy.
In addition, because the signs and symptoms of post-polio syndrome are similar to those of other disorders, your doctor will attempt to exclude other possible causes, such as arthritis, fibromyalgia, chronic fatigue syndrome and scoliosis.
Tests to rule out other conditions
Because there are no tests that confirm a post-polio syndrome diagnosis, your doctor may use certain tests to rule out other conditions, including:
-
Electromyography (EMG) and nerve conduction studies. Electromyography measures the tiny electrical discharges produced in muscles. A thin-needle electrode is inserted into the muscles to be studied. An instrument records the electrical activity in your muscle at rest and as you contract the muscle.
In a variation of EMG called nerve conduction studies, two electrodes are taped to your skin above a nerve to be studied. A small shock is passed through the nerve to measure the speed of nerve signals. These tests help identify and exclude conditions such as an abnormal condition of your nerves (neuropathy) and a muscle tissue disorder (myopathy).
- Imaging. Your doctor might recommend an MRI or CT scan to see images of your brain and spinal cord. These tests can help exclude spinal disorders, such as the degenerative spine condition spondylosis or narrowing of your spinal column that puts pressure on your nerves (spinal stenosis).
- Muscle biopsy. A muscle biopsy might be done to help your doctor look for evidence of another condition that could be causing the weakness.
- Blood tests. People with post-polio syndrome usually have normal blood test results. Abnormal blood test results could indicate another underlying problem that's causing your symptoms.
A noninvasive test that shows promise for evaluating the severity of post-polio syndrome and monitoring its progression is muscle ultrasound, which uses sound waves to create images of muscles. More study is needed.
Treatment
There's no one treatment for the various signs and symptoms of post-polio syndrome. The goal of treatment is to manage your symptoms and help make you as comfortable and independent as possible. Here are some treatment options that may help manage your post-polio syndrome symptoms:
- Energy conservation. This involves pacing your physical activity and resting frequently to reduce fatigue. Assistive devices — such as a cane, walker, wheelchair or motor scooter — can help you conserve energy. Having a shower grab bar or raised toilet seat installed also might help. A therapist can show you ways to breathe that help conserve energy.
-
Physical therapy. Your doctor or therapist may prescribe exercises for you that strengthen your muscles without fatiguing them. These usually include less strenuous activities, such as swimming or water aerobics, that you perform every other day at a relaxed pace.
Exercising to maintain fitness is important, but avoid overusing your muscles and joints and exercising to the point of pain or fatigue.
- Speech therapy. A speech therapist can show you ways to compensate for swallowing difficulties. Voice strengthening exercises also might be helpful.
- Sleep disorder treatment. You might need to change your sleeping patterns, such as avoiding sleeping on your back, or use a device that helps open your airway when you sleep. If you have restless legs syndrome, treatment for that disorder may help improve sleep quality and reduce fatigue.
- Medications. Pain relievers — such as aspirin, acetaminophen (Tylenol, others) and ibuprofen (Advil, Motrin IB, others) — might ease muscle and joint pain.
Other possible treatment options may include the anticonvulsant drug gabapentin (Neurontin, Gralise), which is often used to treat nerve pain. Chronic opioid pain medications generally shouldn't be used due to their long-term risks. You and your doctor should discuss the right treatment plan for you to manage your pain and symptoms.
Self care
Having to deal again with an illness you thought was in the past can be discouraging or even overwhelming at times. Recovering from the initial illness required drive and determination, but now the late effects of polio require you to rest and conserve your energy.
Here are some suggestions:
- Limit activities that cause pain or fatigue. Moderation is key. Overdoing it on a good day can lead to several subsequent bad days.
- Stay warm. Cold increases muscle fatigue. Keep your home at a comfortable temperature and dress in layers, especially when you go out.
- Avoid falls. Get rid of throw rugs and loose clutter on the floor, wear good shoes, and avoid slippery or icy surfaces.
- Maintain a healthy lifestyle. Eat a balanced diet, stop smoking and decrease caffeine intake to keep fit, breathe easier and sleep better.
- Protect your lungs. If your breathing is impaired, watch for signs of a developing respiratory infection and have it treated promptly. Don't smoke, and stay current with your flu and pneumonia vaccines.
Coping and support
Dealing with the fatigue and weakness of post-polio syndrome can be difficult physically and psychologically. You might need to rely on your friends and family. Don't hesitate to tell them what kind of help you need.
Consider joining a support group for people with post-polio syndrome. Sometimes talking things over with people who have similar problems can help you cope. Ask your doctor about support groups in your area.
Preparing for your appointment
You're likely to start by seeing your family doctor. However, you'll likely be referred to a doctor who specializes in nervous system disorders (neurologist).
Here's some information to help you get ready for your appointment.
What you can do
Make a list of:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment, and when they began
- Key personal information, including major stresses or recent life changes, medical history, and family medical history
- All medications, vitamins or other supplements you take, including doses
- Questions to ask your doctor
For post-polio syndrome, basic questions to ask your doctor include:
- What is likely causing my symptoms?
- Are there other possible causes?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What treatments are available? Which do you recommend?
- I have other health conditions. How can I best manage them together?
- Are there activity restrictions I need to follow?
- Will I become incapacitated?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you questions, including:
- Have you ever had polio? If so, when?
- How severe was your polio infection?
- What areas of your body were affected by polio?
- After the polio infection, were you left with persistent weakness?
- Have your symptoms been continuous or occasional?
- What, if anything, seems to improve your symptoms?
- Does anything appear to worsen your symptoms?



