Enlarged heart
Overview
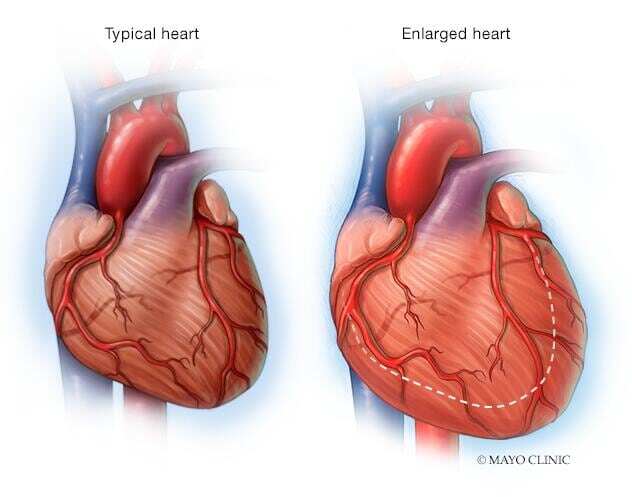
An enlarged heart (cardiomegaly) isn't a disease, but rather a sign of another condition.
The term "cardiomegaly" refers to an enlarged heart seen on any imaging test, including a chest X-ray. Other tests are then needed to diagnose the condition that's causing the enlarged heart.
Heart damage and certain types of heart disease can cause an enlarged heart. Sometimes short-term stress on the body, such as pregnancy, can cause the heart to get larger. Depending on the condition, an enlarged heart may be temporary or permanent.
Treatment for an enlarged heart may include medications, medical procedures or surgery.
Symptoms
In some people, an enlarged heart (cardiomegaly) causes no signs or symptoms. Others may have these signs and symptoms of cardiomegaly:
- Shortness of breath, especially while lying flat
- Waking up short of breath
- Irregular heart rhythm (arrhythmia)
- Swelling (edema) in the belly or in the legs
When to see a doctor
An enlarged heart may be easier to treat when it's detected early. Talk to your health care provider if you have concerns about your heart.
Call 911 or your local emergency number if you have signs and symptoms of a potential heart attack:
- Chest pain
- Discomfort in other areas of the upper body, including one or both arms, the back, neck, jaw, or stomach
- Severe shortness of breath
- Fainting
Causes
An enlarged heart (cardiomegaly) can be caused by damage to the heart muscle or any condition that makes the heart pump harder than usual, including pregnancy. Sometimes the heart gets larger and becomes weak for unknown reasons. This condition is called idiopathic cardiomyopathy.
Conditions associated with an enlarged heart include:
- Heart condition present at birth (congenital heart defect). Problems with the structure and function of the heart can cause the heart muscle to get larger and weak.
- Damage from a heart attack. Scarring and other structural heart damage can make it harder for the heart to pump enough blood to the body. The strain can lead to heart swelling and eventual heart failure.
- Diseases of the heart muscle (cardiomyopathy). Cardiomyopathy often makes the heart rigid or thick. It can make it harder for the heart to pump blood.
- Fluid buildup in the sac around the heart (pericardial effusion). A collection of fluid in the sac that contains the heart can cause heart enlargement that can be seen on a chest X-ray.
- Heart valve disease. Four valves in the heart keep blood flowing in the right direction. Disease or damage to any of the valves may interrupt blood flow and cause the heart chambers to get larger.
- High blood pressure (hypertension). If you have high blood pressure, the heart may have to pump harder to deliver blood to the rest of the body. The strain can cause the heart muscle to grow larger and become weak.
- High blood pressure in the arteries in the lungs (pulmonary hypertension). The heart has to work harder to move blood between the lungs and the heart. The strain may lead to thickening or enlargement of the right side of the heart.
- Low red blood cell count (anemia). In anemia, there's a lack of healthy red blood cells to carry proper levels of oxygen to the body's tissues. The heart must pump more blood to make up for the lack of oxygen in the blood.
- Thyroid disorders. Both an underactive thyroid gland (hypothyroidism) and an overactive thyroid gland (hyperthyroidism) can lead to heart problems, including an enlarged heart.
- Too much iron in the body (hemochromatosis). Iron can build up in various organs, including the heart. This can cause the lower left heart chamber to swell.
- Unusual protein deposits in the heart (cardiac amyloidosis). This rare disease causes a protein called amyloid to collect in the blood and get stuck in body organs, including the heart. Amyloid protein deposits in the heart cause an irreversible thickening of the heart wall. The heart has to work harder to fill with blood.
- Aerobic exercise. In some athletes, the heart becomes enlarged as a response to frequent and prolonged exercise. Usually, this type of enlarged heart isn't considered a disease and doesn't need treatment.
- Fat around the heart. Some people have extra fat around the heart that can appear on a chest X-ray. Unless there are other heart conditions associated, no treatment is necessary.
Risk factors
Things that can increase the risk of an enlarged heart (cardiomegaly) include:
- A family history of heart muscle disease (cardiomyopathy). Some types of cardiomyopathy run in families. Tell your health care provider if a parent or sibling has a history of a thick, rigid or enlarged heart.
- High blood pressure. This means having a blood pressure measurement higher than 140/90 millimeters of mercury.
- Heart diseases. Any problem affecting the heart, including congenital heart defects or heart valve disease, may lead to heart enlargement. It's important to follow a healthy lifestyle and have regular health checkups to manage heart disease.
Complications
The risk of complications from an enlarged heart depends on the part of the heart affected and the cause. Complications of an enlarged heart can include:
- Heart failure. Heart failure may occur if the left lower heart chamber (left ventricle) becomes enlarged. In heart failure, the heart can't pump the proper amount of blood throughout the body.
- Blood clots. Blood clots may form in the lining of the heart. A blood clot that forms on the right side of the heart can travel to the lungs (pulmonary embolism). If a clot blocks blood flow, you could have a heart attack or stroke.
- Leaky heart valve (regurgitation). Heart enlargement may prevent the mitral and tricuspid heart valves from closing, causing blood to leak backward. The interrupted blood flow creates a sound called a heart murmur. Although not necessarily harmful, heart murmurs should be monitored by a health care provider.
- Cardiac arrest and sudden death. An enlarged heart may cause the heart to beat too fast or too slow. The irregular heartbeat (arrhythmia) may lead to fainting, cardiac arrest or sudden death.
Prevention
Tell your health care provider if anyone in your family has or had cardiomyopathy or other health conditions that caused an enlarged heart. When diagnosed early, proper treatment of the underlying condition may prevent the enlarged heart from getting worse.
Following a heart-healthy lifestyle can help prevent or manage some conditions that can lead to an enlarged heart. Take these steps to help prevent an enlarged heart:
- Monitor and manage high blood pressure, high cholesterol and diabetes.
- Take any prescribed medications as directed.
- Eat a nutritious, balanced diet.
- Get regular exercise.
- Avoid or limit alcohol.
- Don't smoke.
- Don't use illegal drugs.
Diagnosis
To diagnose an enlarged heart, a health care provider will usually do a physical exam and ask questions about your symptoms and medical history.
Tests that may be done to help diagnose an enlarged heart (cardiomyopathy) and its cause include:
- Blood tests. Blood tests may help confirm or rule out conditions that can cause heart enlargement. If an enlarged heart occurs with chest pain or other signs of a heart attack, blood tests may be done to check the levels of substances in the blood caused by heart muscle damage.
- Chest X-ray. A chest X-ray can help show the condition of the lungs and heart. If the heart is enlarged on an X-ray, other tests will usually be needed to determine whether the enlargement is real and to find the cause.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which displays the test results. An ECG can show if the heart is beating too fast or too slow. A health care provider can look at signal patterns for signs of a thickened heart muscle (hypertrophy).
- Echocardiogram. This noninvasive test uses sound waves to create images of the heart's size, structure and motion. An echocardiogram shows blood flow through the heart chambers and helps determine how well the heart is working.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is monitored. Exercise tests help reveal how the heart responds to physical activity. If you're unable to exercise, you might be given medications that mimic the effect of exercise on your heart.
-
Cardiac CT scan or MRI. During a cardiac CT scan, you usually lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest.
In a cardiac MRI, you typically lie on a table inside a long tubelike machine that uses a magnetic field and radio waves to produce signals that create images of your heart.
- Cardiac catheterization. A health care provider threads a thin tube (catheter) through a blood vessel in the arm or groin to an artery in the heart and injects dye through the catheter. This makes the heart arteries show up more clearly on an X-ray. During a cardiac catheterization, pressure within the chambers of the heart can be measured to see how forcefully blood pumps through the heart. Sometimes a small piece of heart tissue is removed for examination (biopsy).
Treatment
Treatment of an enlarged heart (cardiomegaly) depends on what is causing the heart problem.
Medications
If cardiomyopathy or another type of heart condition is the cause of an enlarged heart, a health care provider may recommend medications, including:
- Diuretics. These drugs reduce the amount of sodium and water in the body, which can help lower blood pressure.
- Other blood pressure drugs. Beta blockers, angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) may be used to lower blood pressure and improve heart function.
- Blood thinners. Blood-thinning medications (anticoagulants) may be given to reduce the risk of blood clots that could cause a heart attack or stroke.
- Heart rhythm drugs. Also called anti-arrhythmics, these medications help control the heartbeat.
Surgery or other procedures
If medications aren't enough to treat an enlarged heart, medical devices and surgery may be needed.
Surgery or other procedures to treat an enlarged heart may include:
- Pacemaker. A pacemaker is a small device that's usually implanted near the collarbone. One or more electrode-tipped wires run from the pacemaker through the blood vessels to the inner heart. If the heart rate is too slow or if it stops, the pacemaker sends out electrical impulses that stimulate the heart to beat at a steady rate.
- Implantable cardioverter-defibrillator (ICD). If the enlarged heart is causing serious heart rhythm problems (arrhythmias) or you're at risk of sudden death, a surgeon may implant an ICD. An ICD is a battery-powered unit that's placed under the skin near the collarbone — similar to a pacemaker. One or more electrode-tipped wires from the ICD run through veins to the heart. The ICD continuously monitors the heart rhythm. If the ICD detects an irregular heartbeat, it sends out low- or high-energy shocks to reset the heart rhythm.
- Heart valve surgery. If an enlarged heart is caused by heart valve disease, surgery may be needed to repair or replace the affected valve.
- Coronary bypass surgery. If an enlarged heart is due to a blockage in the coronary arteries, this open-heart surgery may be done to reroute blood flow around a clogged artery.
- Left ventricular assist device (LVAD). If you have heart failure, your health care provider may recommend this implantable mechanical pump to help your heart pump. You may have an LVAD implanted while you wait for a heart transplant or, if you're not a candidate for heart transplant, as a long-term treatment for heart failure.
- Heart transplant. A heart transplant is the final treatment option for an enlarged heart that can't be treated in any other way. Because of the shortage of donor hearts, even people who are critically ill may have a long wait before having a heart transplant.
Self care
If you have an enlarged heart or any type of heart disease, your health care provider will likely recommend following a heart-healthy lifestyle. Such a lifestyle typically includes:
- Reducing or avoiding salt
- Limiting saturated and trans fats
- Eating plenty of vegetables, fruits and whole grain foods
- Avoiding or limiting alcohol and caffeine
- Exercising regularly and managing weight
- Controlling heart disease risk factors, including diabetes, high cholesterol and high blood pressure
Preparing for your appointment
If you think you may have an enlarged heart or are worried about your heart disease risk because of your family history, make an appointment with your health care provider. You may be referred to doctor trained in heart diseases (cardiologist).
Here's some information to help you prepare for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet or fast before tests.
- Write down your symptoms,, including ones that may seem unrelated to an enlarged heart or heart disease.
- Write down key personal information, including a family history of heart disease, stroke, high blood pressure or diabetes, and major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements you're taking, including doses.
- Take a family member or friend along, if possible. Someone who goes with you may remember something you missed or forgot.
- Write down questions to ask your health care provider.
Making a list of questions will help you make the most of your time with your health care provider. For an enlarged heart or heart disease, some basic questions to ask your health care provider include:
- What is likely causing my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What tests do I need?
- What's the best treatment?
- What foods should I eat or avoid?
- What's an appropriate level of physical activity?
- Are there restrictions I should follow?
- How often should I be screened for heart disease? For example, how often do I need a cholesterol test?
- I have other health conditions. How can I best manage them together?
- Should I see a specialist?
- Should my children be screened for this condition?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed materials I can take? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your health care provider is likely to ask you questions, including:
- When did your symptoms begin?
- Do you always have symptoms or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, makes your symptoms worse?
- What is your typical diet?
- Do you drink alcohol? How much?
- Do you smoke?
- How often do you exercise?
- Have you been diagnosed with other health conditions?
- Do you have a family history of heart disease?



