Osteoporosis
Overview
Osteoporosis causes bones to become weak and brittle — so brittle that a fall or even mild stresses such as bending over or coughing can cause a break. Osteoporosis-related breaks most commonly occur in the hip, wrist or spine.
Bone is living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn't keep up with the loss of old bone.
Osteoporosis affects men and women of all races. But white and Asian women, especially older women who are past menopause, are at highest risk. Medicines, healthy diet and weight-bearing exercise can help prevent bone loss or strengthen already weak bones.
Symptoms
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
- Back pain, caused by a broken or collapsed bone in the spine.
- Loss of height over time.
- A stooped posture.
- A bone that breaks much more easily than expected.
When to see a doctor
You might want to talk to your health care provider about osteoporosis if you went through early menopause or took corticosteroids for several months at a time, or if either of your parents had hip fractures.
Causes
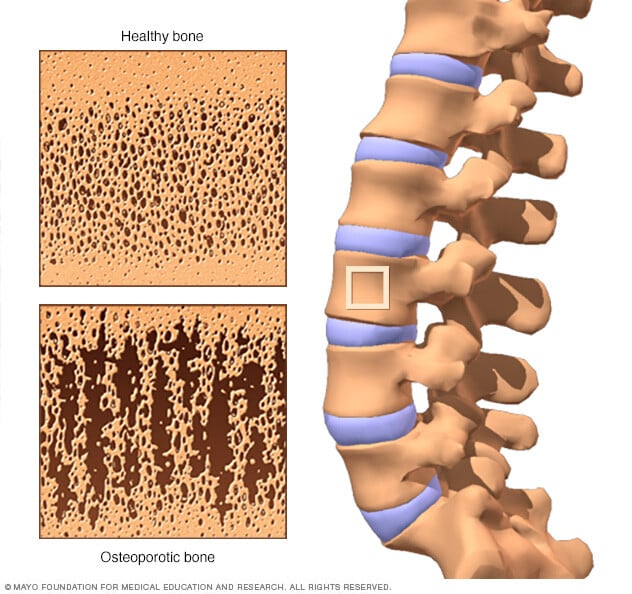
Your bones are in a constant state of renewal — new bone is made and old bone is broken down. When you're young, your body makes new bone faster than it breaks down old bone and your bone mass increases. After the early 20s this process slows, and most people reach their peak bone mass by age 30. As people age, bone mass is lost faster than it's created.
How likely you are to develop osteoporosis depends partly on how much bone mass you attained in your youth. Peak bone mass is partly inherited and varies also by ethnic group. The higher your peak bone mass, the more bone you have "in the bank" and the less likely you are to develop osteoporosis as you age.
Risk factors
A number of factors can increase the likelihood that you'll develop osteoporosis — including your age, race, lifestyle choices, and medical conditions and treatments.
Unchangeable risks
Some risk factors for osteoporosis are out of your control, including:
- Your sex. Women are much more likely to develop osteoporosis than are men.
- Age. The older you get, the greater your risk of osteoporosis.
- Race. You're at greatest risk of osteoporosis if you're white or of Asian descent.
- Family history. Having a parent or sibling with osteoporosis puts you at greater risk, especially if your mother or father fractured a hip.
- Body frame size. Men and women who have small body frames tend to have a higher risk because they might have less bone mass to draw from as they age.
Hormone levels
Osteoporosis is more common in people who have too much or too little of certain hormones in their bodies. Examples include:
- Sex hormones. Lowered sex hormone levels tend to weaken bone. The fall in estrogen levels in women at menopause is one of the strongest risk factors for developing osteoporosis. Treatments for prostate cancer that reduce testosterone levels in men and treatments for breast cancer that reduce estrogen levels in women are likely to accelerate bone loss.
- Thyroid problems. Too much thyroid hormone can cause bone loss. This can occur if your thyroid is overactive or if you take too much thyroid hormone medicine to treat an underactive thyroid.
- Other glands. Osteoporosis has also been associated with overactive parathyroid and adrenal glands.
Dietary factors
Osteoporosis is more likely to occur in people who have:
- Low calcium intake. A lifelong lack of calcium plays a role in the development of osteoporosis. Low calcium intake contributes to diminished bone density, early bone loss and an increased risk of fractures.
- Eating disorders. Severely restricting food intake and being underweight weakens bone in both men and women.
- Gastrointestinal surgery. Surgery to reduce the size of your stomach or to remove part of the intestine limits the amount of surface area available to absorb nutrients, including calcium. These surgeries include those to help you lose weight and for other gastrointestinal disorders.
Steroids and other medicines
Long-term use of oral or injected corticosteroid medicines, such as prednisone and cortisone, interferes with the bone-rebuilding process. Osteoporosis has also been associated with medications used to combat or prevent:
- Seizures.
- Gastric reflux.
- Cancer.
- Transplant rejection.
Medical problems
The risk of osteoporosis is higher in people who have certain medical problems, including:
- Celiac disease.
- Inflammatory bowel disease.
- Kidney or liver disease.
- Cancer.
- Multiple myeloma.
- Rheumatoid arthritis.
Lifestyle choices
Some bad habits can increase your risk of osteoporosis. Examples include:
- Sedentary lifestyle. People who spend a lot of time sitting have a higher risk of osteoporosis than do those who are more active. Any weight-bearing exercise and activities that promote balance and good posture are good for your bones, but walking, running, jumping, dancing and weightlifting seem particularly helpful.
- Excessive alcohol consumption. Regular consumption of more than two alcoholic drinks a day increases the risk of osteoporosis.
- Tobacco use. The exact role tobacco plays in osteoporosis isn't clear, but it has been shown that tobacco use contributes to weak bones.
Complications
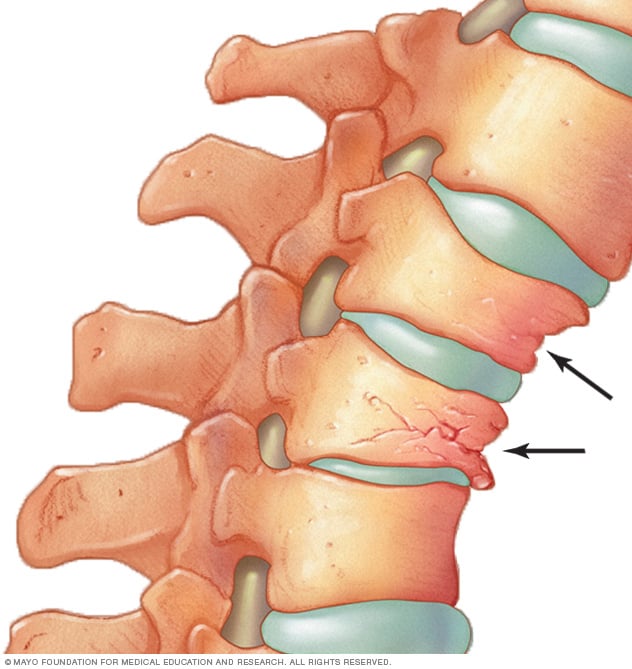
Bone breaks, particularly in the spine or hip, are the most serious complications of osteoporosis. Hip fractures often are caused by a fall and can result in disability and even an increased risk of death within the first year after the injury.
In some cases, broken bones in the spine can occur even if you haven't fallen. The bones that make up your spine, called vertebrae, can weaken to the point of collapsing, which can result in back pain, lost height and a hunched-forward posture.
Prevention
Good nutrition and regular exercise are essential for keeping your bones healthy throughout your life.
Calcium
Men and women between the ages of 18 and 50 need 1,000 milligrams of calcium a day. This daily amount increases to 1,200 milligrams when women turn 50 and men turn 70.
Good sources of calcium include:
- Low-fat dairy products.
- Dark green leafy vegetables.
- Canned salmon or sardines with bones.
- Soy products, such as tofu.
- Calcium-fortified cereals and orange juice.
If you find it difficult to get enough calcium from your diet, consider taking calcium supplements. However, too much calcium has been linked to kidney stones. Although yet unclear, some experts suggest that too much calcium, especially in supplements, can increase the risk of heart disease.
The Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine recommends that total calcium intake, from supplements and diet combined, should be no more than 2,000 milligrams daily for people older than 50.
Vitamin D
Vitamin D improves the body's ability to absorb calcium and improves bone health in other ways. People can get some of their vitamin D from sunlight, but this might not be a good source if you live in a high latitude, if you're housebound, or if you regularly use sunscreen or avoid the sun because of the risk of skin cancer.
Dietary sources of vitamin D include cod liver oil, trout and salmon. Many types of milk and cereal have been fortified with vitamin D.
Most people need at least 600 international units (IU) of vitamin D a day. That recommendation increases to 800 IU a day after age 70.
People without other sources of vitamin D and especially with limited sun exposure might need a supplement. Most multivitamin products contain between 600 and 800 IU of vitamin D. Up to 4,000 IU of vitamin D a day is safe for most people.
Exercise
Exercise can help you build strong bones and slow bone loss. Exercise will benefit your bones no matter when you start, but you'll gain the most benefits if you start exercising regularly when you're young and continue to exercise throughout your life.
Combine strength training exercises with weight-bearing and balance exercises. Strength training helps strengthen muscles and bones in your arms and upper spine. Weight-bearing exercises — such as walking, jogging, running, stair climbing, skipping rope, skiing and impact-producing sports — affect mainly the bones in your legs, hips and lower spine. Balance exercises such as tai chi can reduce your risk of falling especially as you get older.
Diagnosis
Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of mineral in your bones. During this painless test, you lie on a padded table as a scanner passes over your body. In most cases, only certain bones are checked — usually in the hip and spine.
Treatment
Treatment recommendations are often based on an estimate of your risk of breaking a bone in the next 10 years using information such as the bone density test. If your risk isn't high, treatment might not include medication and might focus instead on modifying risk factors for bone loss and falls.
Bisphosphonates
For both men and women at increased risk of broken bones, the most widely prescribed osteoporosis medications are bisphosphonates. Examples include:
- Alendronate (Binosto, Fosamax).
- Risedronate (Actonel, Atelvia).
- Ibandronate.
- Zoledronic acid (Reclast, Zometa).
Side effects include nausea, abdominal pain and heartburn-like symptoms. These are less likely to occur if the medicine is taken properly. Intravenous forms of bisphosphonates don't cause stomach upset but can cause fever, headache and muscle aches.
A very rare complication of bisphosphonates is a break or crack in the middle of the thighbone. A second rare complication is delayed healing of the jawbone, called osteonecrosis of the jaw. This can occur after an invasive dental procedure, such as removing a tooth.
Denosumab
Compared with bisphosphonates, denosumab (Prolia, Xgeva) produces similar or better bone density results and reduces the chance of all types of breaks. Denosumab is delivered via a shot under the skin every six months.
Similar to bisphosphonates, denosumab has the same rare complication of causing breaks or cracks in the middle of the thighbone and osteonecrosis of the jaw. If you take denosumab, you might need to continue to do so indefinitely. Recent research indicates there could be a high risk of spinal column fractures after stopping the drug.
Hormone-related therapy
Estrogen, especially when started soon after menopause, can help maintain bone density. However, estrogen therapy can increase the risk of breast cancer and blood clots, which can cause strokes. Therefore, estrogen is typically used for bone health in younger women or in women whose menopausal symptoms also require treatment.
Raloxifene (Evista) mimics estrogen's beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen. Taking this drug can reduce the risk of some types of breast cancer. Hot flashes are a possible side effect. Raloxifene also may increase your risk of blood clots.
In men, osteoporosis might be linked with a gradual age-related decline in testosterone levels. Testosterone replacement therapy can help improve symptoms of low testosterone, but osteoporosis medications have been better studied in men to treat osteoporosis and thus are recommended alone or in addition to testosterone.
Bone-building medicines
If you have severe osteoporosis or if the more common treatments for osteoporosis don't work well enough, your doctor might suggest trying:
- Teriparatide (Bonsity, Forteo). This powerful drug is similar to parathyroid hormone and stimulates new bone growth. It's given by daily injection under the skin for up to two years.
- Abaloparatide (Tymlos) is another drug similar to parathyroid hormone. This drug can be taken for only two years.
- Romosozumab (Evenity). This is the newest bone-building medicine to treat osteoporosis. It is given as an injection every month at your doctor's office and is limited to one year of treatment.
After you stop taking any of these bone-building medications, you generally will need to take another osteoporosis drug to maintain the new bone growth.
Lifestyle and home remedies
These suggestions might help reduce your risk of developing osteoporosis or breaking bones:
- Don't smoke. Smoking increases rates of bone loss and the chance of fracture.
- Limit alcohol. Consuming more than two alcoholic drinks a day may decrease bone formation. Being under the influence of alcohol also can increase your risk of falling.
- Prevent falls. Wear low-heeled shoes with nonslip soles and check your house for electrical cords, area rugs and slippery surfaces that might cause you to fall. Keep rooms brightly lit, install grab bars just inside and outside your shower door, and make sure you can get into and out of your bed easily.
Preparing for an appointment
Your health care team might suggest bone density testing. Screening for osteoporosis is recommended for all women over age 65. Some guidelines also recommend screening men by age 70, especially if they have health issues likely to cause osteoporosis. If you have a broken bone after a minor force injury, such as a simple fall, bone density testing may be important to assess your risk of more breaks.
If the test results show very low bone density or you have other complex health issues, you might be referred to a provider who specializes in metabolic disorders, called an endocrinologist, or a provider who specializes in diseases of the joints, muscles or bones, called a rheumatologist.
Here's some information to help you get ready for your appointment.
What you can do
- Write down symptoms you've noticed, though it's possible you may not have any.
- Write down key personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements that you take or have taken, including doses. It's especially helpful if you record the type and dose of calcium and vitamin D supplements, because many different preparations are available. If you're not sure what information your doctor might need, take the bottles with you or take a picture of the label with your smartphone and share it with your doctor.
- Write down questions to ask your health care provider.
For osteoporosis, basic questions to ask your provider include:
- Do I need to be screened for osteoporosis?
- What treatments are available, and which do you recommend?
- What side effects might I expect from treatment?
- Are there alternatives to the treatment you're suggesting?
- I have other health problems. How can I best manage them together?
- Do I need to restrict my activities?
- Do I need to change my diet?
- Do I need to take supplements?
- Is there a physical therapy program that would benefit me?
- What can I do to prevent falls?
Don't hesitate to ask other questions.
What to expect from your doctor
Your provider is likely to ask you questions, such as:
- Have you broken bones?
- Have you gotten shorter?
- How is your diet, especially your dairy intake? Do you think you get enough calcium? Vitamin D?
- How often do you exercise? What type of exercise do you do?
- How is your balance? Have you fallen?
- Do you have a family history of osteoporosis?
- Has a parent broken a hip?
- Have you ever had stomach or intestinal surgery?
- Have you taken corticosteroid medicines, including prednisone, cortisone, as pills, injections or creams?