Nasal polyps
Overview
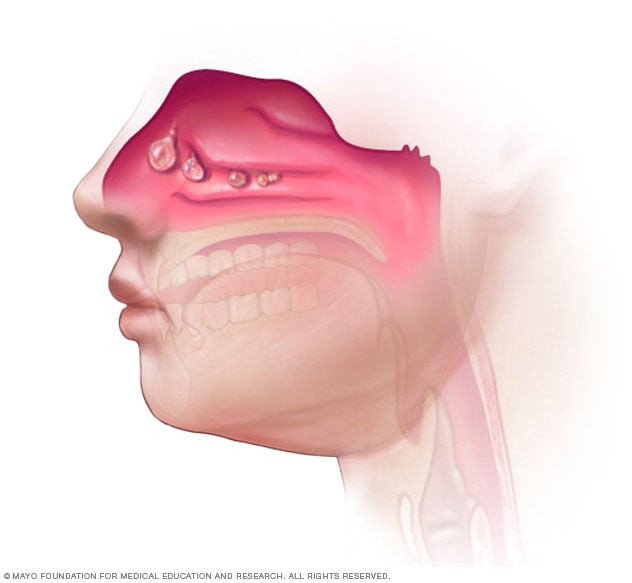
Nasal polyps are painless growths inside the nose or the hollow areas inside the bones of the face, also known as sinuses. Nasal polyps aren't cancer.
Small nasal polyps might not cause symptoms. Larger growths or groups of nasal polyps can block the nose. They can lead to breathing problems, not being able to smell and infections.
Nasal polyps can affect anyone. But they're more common in young and middle-aged adults. Medicines can often shrink nasal polyps or get rid of them. But surgery might be needed to remove them. Even after treatment, nasal polyps often come back.
Symptoms
Nasal polyps are linked to irritation and swelling, also called inflammation, of the inside of the nose and sinuses that lasts more than 12 weeks. This is known as chronic sinusitis. But it's possible to have chronic sinusitis without getting nasal polyps.
People who have small nasal polyps might not know they have them. But having more than one polyp or having a large polyp can block the nose.
Common symptoms of chronic sinusitis with nasal polyps include:
- Runny, stuffy nose.
- Mucus running down the throat, also known as postnasal drip.
- Not being able to smell.
- Not being able to taste.
- Facial pain or headache.
- Pain in the teeth.
- A sense of pressure over the forehead and face.
- Snoring.
When to see a doctor
See a health care provider for symptoms that last more than 10 days. Symptoms of chronic sinusitis and nasal polyps are like those of many other illnesses, including the common cold.
Seek medical care right away or call 911 or your local emergency number if you have:
- Symptoms that quickly get worse.
- Seeing double or other vision changes.
- Swollen forehead.
- Pain or swelling around the eyes.
- A bad headache that keeps getting worse.
- Stiff neck.
Causes
Experts don't know what causes nasal polyps. They don't know why some people get nasal polyps and others don't.
Risk factors
Infections, allergies or any condition that causes long-term inflammation in the nose or sinuses can increase the risk of having nasal polyps.
Conditions often linked to nasal polyps include:
- Asthma.
- Aspirin sensitivity.
- Cystic fibrosis.
- Dental infections.
- Lack of vitamin D.
Having a family history of nasal polyps also might increase the risk.
Complications
One of the most common complications of chronic sinusitis with nasal polyps is making asthma worse.
Prevention
The following might help lower the chances of getting nasal polyps or having nasal polyps come back after treatment:
- Manage allergies and asthma. Follow your treatment plan. Be sure symptoms are controlled. See your health care provider if they're not.
- Avoid things that can irritate the nose. These include tobacco smoke, chemical fumes and dust. If you smoke, talk to your health care provider about ways to quit.
- Wash your hands often and well. This is one of the best ways to protect against infections that can cause irritation and swelling of the nose and sinuses.
- Use a machine that adds moisture to the air, known as a humidifier. This might help prevent the nose from getting stuffy and irritated. Clean the humidifier as directed to keep bacteria from growing.
-
Use a nasal rinse. Rinsing the inside of the nose with a saltwater spray or nasal wash might help remove what irritates it.
You can buy saltwater sprays and nasal wash kits without a prescription. Nasal wash kits come with a neti pot or squeeze bottle and directions for how to use them.
Use water that's distilled or sterile or has been boiled for one minute and cooled. The water can also be filtered using a filter with an absolute pore size of 1 micron or smaller. Rinse the pot or bottle after each use with the distilled, sterile, previously boiled or filtered water and leave it open to dry.
Diagnosis
A diagnosis of nasal polyps starts with symptoms, a medical history and a physical exam.
Tests to diagnose nasal polyps might include:
- Nasal endoscopy. This involves using a narrow tube with a lighted lens or tiny camera to look at the inside of the nose.
- Imaging studies. CT scans can show the size of polyps deep in the sinuses and where they are. These studies can also help rule out other reasons the nose is blocked.
-
Allergy tests. Skin tests can show if allergies are causing ongoing inflammation. With a skin prick test, tiny drops of allergy-causing agents are pricked into the skin of the forearm or upper back. A health care provider then watches the skin for allergic reactions.
If a skin test can't be done, a blood test can screen for allergies.
-
Test for cystic fibrosis. A child who has nasal polyps might have cystic fibrosis. Cystic fibrosis affects the cells that make mucus, sweat and the juices that help food digest. It's an inherited condition.
A test for cystic fibrosis is a sweat test. A chemical put on the skin causes the area to sweat. The test shows if the sweat is saltier than most people's sweat is.
- Blood tests. These can look for a condition linked to nasal polyps, such as allergies or problems with the immune system.
Treatment
Chronic sinusitis, with or without polyps, is hard to clear up. Treatment depends on the cause of the swelling and irritation. The goal is to lessen symptoms and improve life.
Medicines
Treatments might include:
- Nasal steroids. These nasal sprays include fluticasone (Flonase Allergy Relief, Xhance), budesonide (Rhinocort), mometasone (Nasonex 24hr Allergy), triamcinolone (Nasacort Allergy 24HR), beclomethasone (Beconase AQ, Qnasl) and ciclesonide (Omnaris, Zetonna).
-
Steroids taken by mouth. Some nasal polyps can block nasal sprays. If so, taking steroids in pill form such as prednisone might help. Steroids taken by mouth also might be given to shrink polyps before surgery.
The pills can be taken alone or with a nasal spray. Because oral steroids can cause serious side effects, health care providers generally prescribe them only for a short time.
Steroids given as shots may be used if nasal polyps are severe.
- Biologic medicines. Biologics work by aiming at certain cells or proteins to lessen irritation and swelling. These might be used for people whose nasal polyps keep coming back. In the United States, dupilumab (Dupixent), mepolizumab (Nucala) and omalizumab (Xolair) have been approved for treatment of chronic sinusitis with nasal polyps.
-
Other medicines. Other prescription medicines can treat conditions that lead to long-term swelling and inflammation in the nose. These might include medicines to treat allergies, also known as antihistamines, and antibiotics to treat infection.
A treatment known as aspirin desensitization might help people with nasal polyps and asthma who react badly to aspirin. An allergy specialist oversees the treatment. The treatment involves taking a little more aspirin bit by bit to help the body get used to taking aspirin.
Surgery to remove the polyps might come before aspirin desensitization. Desensitization might be followed by daily aspirin therapy.
Surgery
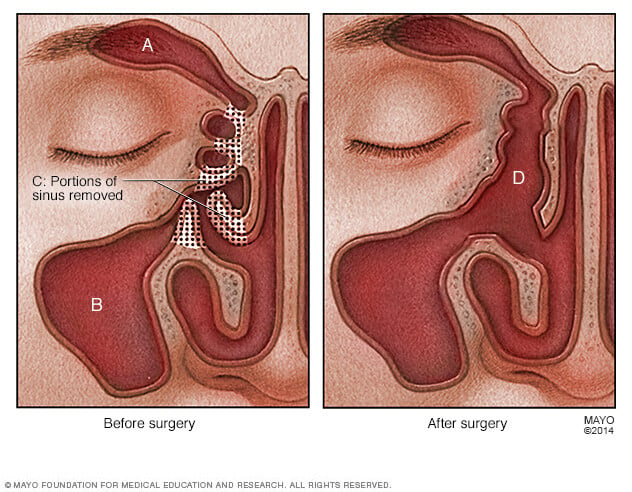
If medicine doesn't shrink or get rid of nasal polyps, endoscopic surgery can remove polyps and correct problems with the sinuses that lead to polyps.
In endoscopic surgery, a surgeon puts a small tube with a lighted lens or tiny camera, also known as an endoscope, through the nostrils into the sinuses. A surgeon then uses tiny tools to remove polyps.
A surgeon can also make the openings to the sinuses larger. This can be done during endoscopic surgery. Or there's a procedure called balloon ostial dilation. This procedure doesn't involve removing tissue from inside the nose.
After surgery, a corticosteroid nasal spray might help keep nasal polyps from coming back. A saltwater rinse can promote healing after surgery.
Preparing for an appointment
You'll likely start by seeing your primary care provider. You might then be referred to an ear, nose and throat (ENT) specialist or an allergy specialist.
Here's some information to help you get ready for your appointment.
What you can do
Ask a family member or friend to go with you, if possible. Having someone with you can help you recall the information you get during the appointment.
Make a list of:
- Your symptoms, even if they seem unrelated to your nose or sinuses, and when they began.
- Other medical information, including other conditions you have.
- All medicines, vitamins and supplements you take, including doses.
- Questions to ask your health care provider.
Some basic questions to ask might include:
- What is likely causing my symptoms?
- What tests do I need?
- What treatment do you suggest?
- Do I need to see a specialist?
- Are there brochures or other printed information I can take have? What websites do you recommend?
Ask other questions you have.
What to expect from your doctor
Your care provider might ask you questions, including:
- When did you last have a cold or sinus infection?
- How often do you have colds or sinus infections?
- Do you have allergies? To what?
- Do you have asthma? How controlled is it?
- Do you often take aspirin or any other pain medicines?
- Do you smoke or are you often around tobacco smoke?
- What kind of work do you do?
- What are your hobbies?
- Have you ever had any sinus or nasal surgery?