Pyloric stenosis
Overview
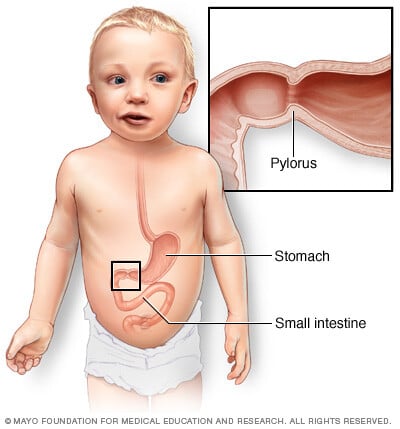
Pyloric stenosis is an uncommon condition in infants that blocks food from entering the small intestine.
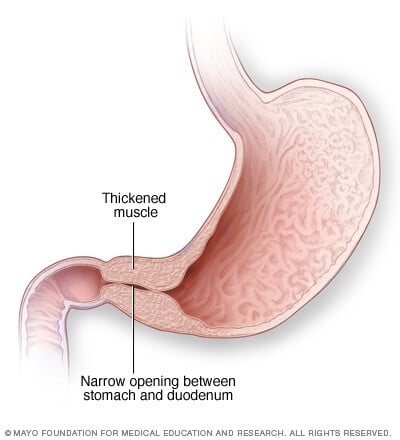
Typically, a muscular valve between the stomach and small intestine holds food in the stomach until it is ready for the next stage in the digestive process. This valve is called the pylorus valve. In pyloric stenosis, the pylorus muscles thicken and become abnormally large, blocking food from reaching the small intestine.
Pyloric stenosis can lead to forceful vomiting, dehydration and weight loss. Babies with pyloric stenosis may seem to be hungry all the time.
Surgery cures pyloric stenosis.
Symptoms
Symptoms of pyloric stenosis usually appear within 3 to 5 weeks after birth. Pyloric stenosis is rare in babies older than 3 months.
Symptoms include:
- Vomiting after feeding. The baby may vomit forcefully, ejecting breast milk or formula up to several feet away. This is known as projectile vomiting. Vomiting might be mild at first. But over time, it becomes more severe as the pylorus opening narrows. The vomit may sometimes contain blood.
- Persistent hunger. Babies who have pyloric stenosis often want to eat soon after vomiting.
- Stomach contractions. You may notice wavelike contractions that ripple across your baby's upper stomach area soon after feeding but before vomiting. These contractions are part of the digestive process known as peristalsis. The contractions are caused by stomach muscles trying to force food through the narrowed pylorus.
- Dehydration. Your baby might cry without tears or become lethargic. You might find yourself changing fewer wet diapers or diapers that aren't as wet as you expect.
- Changes in bowel movements. Since pyloric stenosis prevents food from reaching the intestines, babies with this condition might be constipated.
- Weight problems. Pyloric stenosis can keep a baby from gaining weight, and sometimes can cause weight loss.
When to see a doctor
See your baby's doctor if your baby:
- Projectile vomits after feeding.
- Seems less active or unusually irritable.
- Urinates much less frequently or has noticeably fewer bowel movements.
- Isn't gaining weight or is losing weight.
Causes
The causes of pyloric stenosis are unknown, but genetic and environmental factors might play a role. Pyloric stenosis usually isn't present at birth and probably develops afterward.
Risk factors
Risk factors for pyloric stenosis include:
- Sex. Pyloric stenosis is seen more often in boys, especially firstborn children, than in girls.
- Race and ethnicity. Pyloric stenosis is more common in white and Hispanic children.
- Premature birth. Pyloric stenosis is more common in babies born prematurely than in full-term babies.
- Family history. Studies found higher rates of this disorder among certain families. Pyloric stenosis develops in about 20% of male descendants and 10% of female descendants of mothers who had the condition.
- Smoking during pregnancy. This behavior can nearly double the risk of pyloric stenosis.
- Early antibiotic use. Babies given certain antibiotics in the first weeks of life — erythromycin to treat whooping cough, for example — have an increased risk of pyloric stenosis. In addition, babies born to mothers who took certain antibiotics in late pregnancy may have an increased risk of pyloric stenosis.
- Bottle-feeding. Some studies suggest that bottle-feeding rather than breastfeeding can increase the risk of pyloric stenosis. Most of the people who participated in these studies used formula rather than breast milk, so it isn't clear whether the increased risk is related to formula or the mechanism of bottle-feeding.
Complications
Pyloric stenosis can lead to:
- Failure to grow and develop.
- Dehydration. Frequent vomiting can cause dehydration and a mineral imbalance. These minerals are called electrolytes. Electrolytes help regulate many vital functions.
- Stomach irritation. Repeated vomiting can irritate your baby's stomach and may cause mild bleeding.
- Jaundice. Rarely, a substance secreted by the liver can build up, causing a yellowing of the skin and eyes. This substance is known as bilirubin.
Diagnosis
Your baby's health care provider will start with a physical examination. Sometimes, the provider can feel an olive-shaped lump when examining the baby's belly. This lump is the enlarged pylorus muscles. Wavelike contractions may sometimes be visible when examining the baby's belly, often before the baby starts vomiting.
Your provider also might recommend:
- Blood tests to check for dehydration or electrolyte imbalance or both.
- Ultrasound to view the pylorus and confirm a diagnosis of pyloric stenosis.
- X-rays of your baby's digestive system, if results of the ultrasound aren't clear.
Treatment
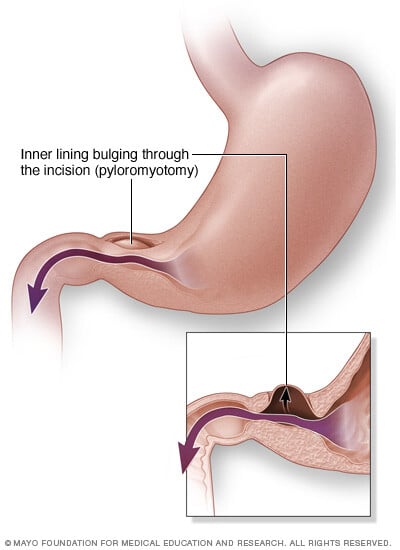
Surgery is needed to treat pyloric stenosis. The procedure, called a pyloromyotomy, is often scheduled on the same day as the diagnosis. If your baby is dehydrated or has an electrolyte imbalance, your baby receives fluids [fluid replacement] before surgery.
In pyloromyotomy, the surgeon cuts only through the outside layer of the thickened pylorus muscle, allowing the inner lining to bulge out. This opens a channel for food to pass through to the small intestine.
Pyloromyotomy is often done using minimally invasive surgery. A slender viewing instrument, called a laparoscope, is inserted through a small incision near the baby's navel. Recovery from a laparoscopic procedure is usually quicker than recovery from traditional surgery. This method also leaves a smaller scar.
After surgery:
- Your baby might be given intravenous fluids for a few hours. You can start feeding your baby again within 12 to 24 hours.
- Your baby might want to feed more often.
- Some vomiting may continue for a few days.
Possible complications from pyloric stenosis surgery include bleeding and infection. However, complications aren't common, and the results of surgery are generally excellent.
Preparing for an appointment
You may be referred to a health care provider who specializes in treating digestive disorders, called a gastroenterologist. Or you may be referred to a pediatric surgeon.
What you can do
- Write down your baby's symptoms, including when and how often your baby vomits, whether the vomit is forcefully projected, and if the vomit appears to be most or just part what the baby has eaten.
- Write down questions to ask your health care provider.
Questions to ask your doctor
- What's the most likely cause of my baby's symptoms?
- What tests does my baby need? Do they require any special preparation?
- What treatments are available? Does my baby need surgery?
- Will there be any feeding restrictions after surgery?
In addition to the questions that you've prepared, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your provider is likely to ask you a few questions. Being ready to answer them may leave time to go over points you want to spend more time on. You may be asked:
- When did your baby first begin experiencing symptoms?
- Are the symptoms continuous or occasional? Do they occur only after eating?
- Does your baby seem hungry after vomiting?
- Does the vomit come out forcefully?
- Does your baby have four or more wet diapers a day?
- Is there blood in your baby's stool?
- What was your baby's last recorded weight?



