Retinal detachment
Overview
Retinal detachment happens when the thin layer of tissue at the back of the eye pulls away from its regular position. This layer of tissue is called the retina. Retinal detachment is an emergency.
Retinal detachment separates the retinal cells from the layer of blood vessels that provides oxygen and nourishment to the eye. The longer retinal detachment goes without treatment, the greater the risk of permanent vision loss in the affected eye.
Symptoms of retinal detachment can include the following: reduced vision, the sudden appearance of dark floating shapes and flashes of light in your vision, and loss of side vision. Contacting an eye doctor, called an ophthalmologist, right away can help save your vision.
Symptoms
Retinal detachment is painless. Often, symptoms are present before a retinal detachment happens or before it has gotten worse. You may notice symptoms such as:
- The sudden appearance of tiny specks or squiggly lines that seem to drift through your field of vision. These are called floaters.
- Flashes of light in one or both eyes. These are called photopsias.
- Blurred vision.
- Side vision, also called peripheral vision, that becomes worse.
- A curtainlike shadow over your field of vision.
When to see a doctor
See a healthcare professional right away if you have any symptoms of retinal detachment. This condition is an emergency that can cause lasting vision loss.
Causes
There are three main types of retinal detachment, and their causes vary:
-
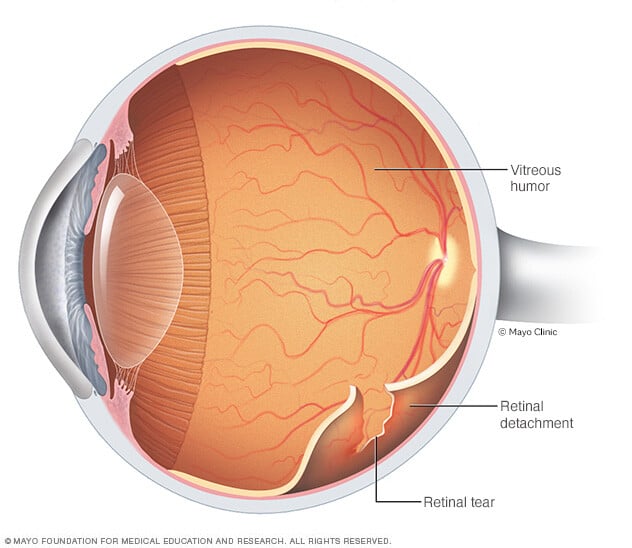
Rhegmatogenous (reg-mu-TOJ-uh-nus). This type of retinal detachment is the most common. A rhegmatogenous detachment is caused by a hole or tear in the retina that lets fluid pass through and collect underneath the retina. This fluid builds up and causes the retina to pull away from underlying tissues. The areas where the retina detaches lose their blood supply and stop working. This causes you to lose vision.
The most common cause of rhegmatogenous detachment is aging. As you age, gel-like material that fills the inside of your eye, called vitreous (VIT-ree-us), may change in texture and shrink or become more liquid. Usually, the vitreous separates from the surface of the retina without any complications. This is a common condition called a posterior vitreous detachment (PVD).
As the vitreous separates or peels off the retina, it may tug on the retina with enough force to create a tear. Most of the time it doesn't. But if a PVD causes a tear and the tear isn't treated, the liquid vitreous can pass through the tear into the space behind the retina. This causes the retina to detach.
- Tractional. This type of detachment can happen when scar tissue grows on the retina's surface. The scar tissue causes the retina to pull away from the back of the eye. Tractional detachment usually is seen in people who have poorly controlled diabetes.
- Exudative. In this type of detachment, fluid builds up beneath the retina, but there are no holes or tears in the retina. Exudative detachment can be caused by age-related macular degeneration, infection, tumors or inflammatory conditions.
Risk factors
The following factors raise your risk of retinal detachment:
- Aging — retinal detachment is more common in people ages 40 to 70.
- Past retinal detachment in one eye.
- Family history of retinal detachment.
- Extreme nearsightedness, also called myopia.
- Past eye surgery, such as cataract removal.
- Past severe eye injury.
- History of other eye disease or condition, including retinoschisis, uveitis or thinning of the peripheral retina called lattice degeneration.
Diagnosis
Diagnosis involves the steps that your healthcare professional takes to find out if retinal detachment is the cause of your symptoms. Your healthcare team may use the following tests and instruments to diagnose retinal detachment:
- Retinal exam. Your healthcare professional may use an instrument with a bright light and special lenses to check the back of your eye, including the retina. This type of device provides a detailed view of your whole eye. It lets your healthcare professional see any retinal holes, tears or detachments.
- Ultrasound imaging. Your healthcare professional may use this test if bleeding has happened in your eye. Bleeding makes it hard to see the retina.
Your healthcare professional likely will check both eyes even if you have symptoms in just one. If a retinal tear is not found at this visit, your healthcare professional may ask you to return within a few weeks. The return visit is done to confirm that your eye has not developed a delayed retinal tear due to the same vitreous detachment. Also, if you have new symptoms, it's important to return to your healthcare professional right away.
Treatment
Surgery is almost always the type of treatment used to repair a retinal tear, hole or detachment. Various techniques are available. Ask your ophthalmologist about the risks and benefits of your treatment options. Together you can decide what treatment or combination of treatments is best for you.
Retinal tears
When the retina has a tear or hole but hasn't yet become detached, your eye surgeon may suggest one of the following treatments. These treatments can help prevent retinal detachment and preserve vision.
- Laser surgery, also called laser photocoagulation or retinopexy. The surgeon directs a laser beam into the eye through the pupil. The laser makes burns around the retinal tear to create scarring that usually "welds" the retina to underlying tissue.
- Freezing, also called cryopexy. Before treatment starts, you're given medicine to numb your eye. Then the surgeon applies a freezing probe to the outer surface of the eye directly over the tear. The freezing causes a scar that helps secure the retina to the eye wall.
Both of these treatments can be done in the eye doctor's office. Most often, you can go home afterward. You'll likely be told not to do activities that might jar the eyes — such as running — for a couple of weeks or so.
Retinal detachment
If your retina has detached, you'll need surgery to repair it. It's ideal to get surgery within days of finding out that your retina has detached. The type of surgery that your surgeon recommends depends on factors such as the location of the retinal detachment and how severe it is.
-
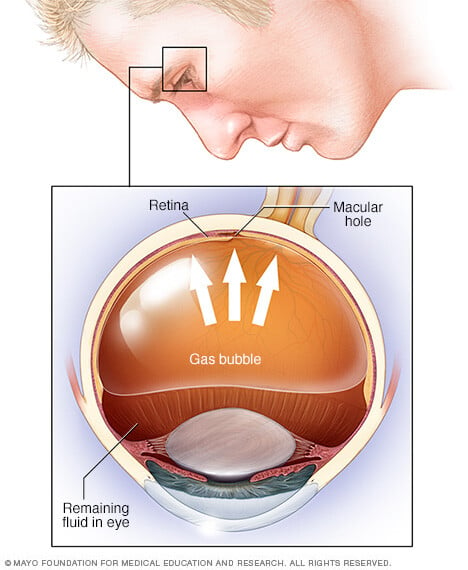
Injecting air or gas into the eye. This surgery is called pneumatic retinopexy (RET-ih-no-pek-see). A surgeon injects a bubble of air or gas into the center part of the eye, also called the vitreous cavity. When positioned properly, the bubble pushes the area of the retina that contains the hole or holes against the wall of the eye. This stops the flow of fluid into the space behind the retina. The surgeon also uses cryopexy or laser photocoagulation during the treatment to create scarring around the retinal break.
Fluid that had collected underneath the retina is absorbed by itself, and the retina can then stick to the wall of the eye. You may need to hold your head in a certain position for up to a week to keep the bubble in the proper position. The bubble goes away on its own in time.
- Indenting the surface of the eye. This surgery is called scleral (SKLAIR-ul) buckling. It involves the surgeon sewing a piece of silicone to the white part of the eye, called the sclera, over the affected area. This surgery indents the wall of the eye and relieves some of the force caused by the vitreous tugging on the retina. The silicone is placed in a way that doesn't block your vision, and it usually remains in place for life. During surgery, cryoretinopexy or laser photocoagulation may be done to help seal tears in the retina. If fluid has collected below the retina, the surgeon may drain it.
-
Draining and replacing the fluid in the eye. This surgery is known as vitrectomy (vih-TREK-tuh-me). The surgeon removes the vitreous along with any tissue that is tugging on the retina. Air, gas or silicone oil is then injected into the vitreous space to help flatten the retina. During surgery, tears in the retina can be sealed with cryoretinopexy or laser photocoagulation. There may be fluid below the retina that needs to be drained.
The air or gas that is injected into the vitreous space is absorbed in time. The vitreous space refills with fluid. If silicone oil was used, it may be removed with surgery months later.
Vitrectomy may be combined with scleral buckling.
After surgery, your vision may take months to get better. You may need a second surgery for successful treatment. Some people never get back all of their lost vision.
Coping and support
Retinal detachment may cause you to lose vision. Depending on your amount of vision loss, your lifestyle might change a lot.
You may find the following ideas useful as you learn to live with impaired vision:
- Get glasses. Your glasses prescription may change after retinal detachment repair, especially if the detachment is treated with a scleral buckle. Get an updated prescription once your eye has healed to make the most of your vision. Request safety lenses to protect your eyes.
- Brighten your home. Have proper light in your home for reading and other activities.
- Make your home safer. Get rid of throw rugs or secure the rugs to the floor with tape to prevent slips and falls. Move electrical cords out of the way from areas where you walk a lot. And place colored tape on the edges of steps. Think about installing lights that turn on when they detect movement.
- Ask for help if you need it. Tell friends and family members about your vision changes so that they can help you.
- Get help from technology. Digital talking books and computer screen readers can help with reading. Other new technology continues to advance.
- Explore driving services. Look into vans and shuttles, volunteer driving networks, or ride-sharing services available in your area for people with impaired vision.
- Talk to others with impaired vision. Take advantage of online networks, support groups and resources for people with impaired vision.
Preparing for an appointment
Here's some information to help you get ready for your appointment.
What you can do
- Be aware of any restrictions before your appointment. At the time you make the appointment, ask if you need to do anything in advance.
- List any symptoms that you have, including those that don't seem related to the reason for which you made the appointment.
- List key personal information, including major stresses and recent life changes.
- List all medicines, vitamins and supplements that you take, including doses.
- Ask a family member or friend to come with you. You may wish to ask someone who could drive you home if your eyes are dilated as a part of your exam. Or this person could write down information from your healthcare team during the appointment.
- List questions to ask your healthcare professional.
For retinal detachment, some basic questions include:
- What's the most likely cause of my symptoms?
- What are other possible causes of my symptoms?
- What tests do I need? Do I need to do anything to prepare for them?
- Is my condition likely short-term or ongoing?
- What are my treatment options, and which do you recommend?
- Are there options aside from the main treatment that you've suggested?
- I have another medical condition. How can I best manage my conditions together?
- Do I need to restrict my activities in any way?
- Do I need to see another specialist?
- Do you have any brochures or other printed material I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
- If I need surgery, how long will recovery take?
- Will I be able to travel after surgery? Will it be safe to travel by plane?
What to expect from your doctor
Your healthcare professional is likely to ask you questions such as:
- When did you first start having symptoms?
- Do you have your symptoms all the time, or do they come and go?
- How severe are your symptoms?
- Have you had any symptoms in your other eye?
- Have you ever had an eye injury?
- Have you ever had eye inflammation?
- Have you ever had eye surgery?
- Do you have any other health conditions such as diabetes?
- Have any of your family members ever had a retinal detachment?



