Essential tremor
Overview
Essential tremor is a nervous system condition, also known as a neurological condition, that causes involuntary and rhythmic shaking. It can affect almost any part of the body, but the trembling occurs most often in the hands, especially when doing simple tasks, such as drinking from a glass or tying shoelaces.
Essential tremor is usually not a dangerous condition, but it typically worsens over time and can be severe in some people. Other conditions don't cause essential tremor, although essential tremor is sometimes confused with Parkinson's disease.
Essential tremor can occur at any age but is most common in people age 40 and older.
Symptoms
Essential tremor symptoms:
- Begin gradually, and usually are more noticeable on one side of the body.
- Worsen with movement.
- Usually occur in the hands first, affecting one hand or both hands.
- Can include a "yes-yes" or "no-no" motion of the head.
- May be aggravated by emotional stress, fatigue, caffeine or temperature extremes.
Essential tremor vs. Parkinson's disease
Many people associate tremors with Parkinson's disease, but the two conditions differ in key ways:
- Timing of tremors. Essential tremor of the hands usually occurs when using the hands. Tremors from Parkinson's disease are most noticeable when the hands are at the sides of the body or resting in the lap.
- Associated conditions. Essential tremor doesn't cause other health problems, but Parkinson's disease is associated with stooped posture, slow movement and dragging the feet when walking. However, people with essential tremor sometimes develop other neurological signs and symptoms, such as an unsteady walk.
- Parts of the body affected. Essential tremor mainly involves the hands, head and voice. Parkinson's disease tremors usually start in the hands, and can affect the legs, chin and other parts of the body.
Causes
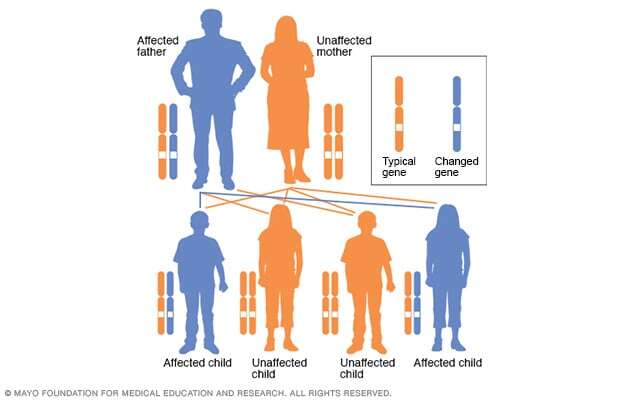
About half the people with essential tremor appear to have an altered gene. This form is referred to as familial tremor. It isn't clear what causes essential tremor in people who don't have familial tremor.
Risk factors
Known risk factors for essential tremor include:
-
Altered gene. The inherited variety of essential tremor, known as familial tremor, is an autosomal dominant disorder. An altered gene from just one parent is needed to pass on the condition.
Anyone who has a parent with an altered gene for essential tremor has a 50% chance of developing the condition.
- Age. Essential tremor is more common in people age 40 and older.
Complications
Essential tremor isn't life-threatening, but symptoms often worsen over time. If the tremors become severe, it might be difficult to:
- Hold a cup or glass without spilling.
- Eat without shaking.
- Put on makeup or shave.
- Talk, if the voice box or tongue is affected.
- Write legibly.
Diagnosis
Diagnosing essential tremor involves a review of your medical history, family history and symptoms and a physical examination.
There are no medical tests to diagnose essential tremor. Diagnosing it is often a matter of ruling out other conditions that could be causing symptoms. To do this, your health care provider may suggest the following tests.
Neurological examination
In a neurological examination, your health care provider tests your nervous system functioning, including checking your:
- Tendon reflexes.
- Muscle strength and tone.
- Ability to feel certain sensations.
- Posture and coordination.
- Gait.
Laboratory tests
Blood and urine may be tested for several factors, including:
- Thyroid disease.
- Metabolic problems.
- Medicine side effects.
- Levels of chemicals that may cause tremor.
Performance tests
To evaluate the tremor itself, your health care provider may ask you to:
- Drink from a glass.
- Hold your arms outstretched.
- Write.
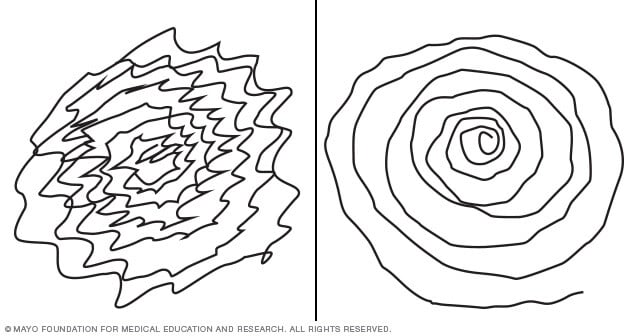
- Draw a spiral.
A health care provider who still is not sure if a tremor is essential tremor or Parkinson's disease might order a dopamine transporter scan. This scan can help the provider tell the difference between the two types of tremor.
Treatment
Some people with essential tremor don't require treatment if their symptoms are mild. But if your essential tremor is making it difficult to work or perform daily activities, discuss treatment options with your health care provider.
Medicines
- Beta blockers. Typically used to treat high blood pressure, beta blockers such as propranolol (Inderal LA, InnoPran XL, Hemangeol) help relieve tremors in some people. Beta blockers may not be an option for people with asthma or certain heart problems. Side effects may include fatigue, lightheadedness or heart problems.
- Anti-seizure medicines. Primidone (Mysoline) may be effective in people who don't respond to beta blockers. Other medicines that might be prescribed include gabapentin (Gralise, Neurontin, Horizant) and topiramate (Topamax, Qudexy XR, others). Side effects include drowsiness and nausea, which usually disappear within a short time.
- Tranquilizers. Health care providers may use benzodiazepines such as clonazepam (Klonopin) to treat people for whom tension or anxiety worsens tremors. Side effects can include fatigue or mild sedation. These medicines should be used with caution because they can be habit-forming.
-
OnabotulinumtoxinA (Botox) injections. Botox injections might be useful in treating some types of tremors, especially head and voice tremors. Botox injections can improve tremors for up to three months at a time.
However, if Botox is used to treat hand tremors, it can cause weakness in the fingers. If Botox is used to treat voice tremors, it can cause a hoarse voice and difficulty swallowing.
Therapy
Health care providers might suggest physical or occupational therapy. Physical therapists can teach you exercises to improve your muscle strength, control and coordination.
Occupational therapists can help you adapt to living with essential tremor. Therapists might suggest adaptive devices to reduce the effect of tremors on your daily activities, including:
- Heavier glasses and utensils.
- Wrist weights.
- Wider, heavier writing tools, such as wide-grip pens.
Nerve stimulation devices
A wearable electronic peripheral nerve stimulation device (Cala Trio) is a newer treatment option for people with essential tremor. The device, which can be worn as a wristband for 40 minutes twice a day, works by stimulating peripheral nerves and muscles to create a muscle response that reduces tremors. Studies have found that the device can bring some improvement for tremors.
Surgery
Surgery might be an option if your tremors are severely disabling, and you don't respond to medicines.
-
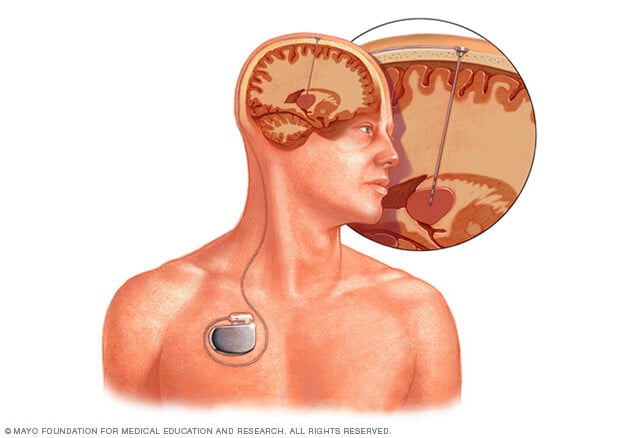
Deep brain stimulation. This is the most common type of surgery for essential tremor. It's generally the preferred procedure in medical centers with significant experience in performing this surgery. It involves putting a long, thin electrical probe into the portion of the brain that causes the tremors, known as the thalamus. A wire from the probe runs under the skin to a pacemaker-like device called a neurostimulator that's implanted in the chest. This device transmits painless electrical pulses to interrupt signals from the thalamus that may be causing the tremors.
Side effects of deep brain stimulation can include equipment malfunction; problems with motor control, speech or balance; headaches; and weakness. Side effects often go away after some time or adjustment of the device.
-
Focused ultrasound thalamotomy. This noninvasive surgery involves using focused sound waves that travel through the skin and skull. The waves generate heat to destroy brain tissue in a specific area of the thalamus to stop a tremor. A surgeon uses magnetic resonance imaging to target the correct area of the brain and to be sure the sound waves are generating the exact amount of heat needed for the procedure.
Focused ultrasound thalamotomy is done on one side of the brain. The surgery affects the other side of the body from the one where it's done.
Focused ultrasound thalamotomy creates a sore that can result in permanent changes to brain function. Some people have experienced altered sensation, trouble with walking or difficulty with movement. However, most complications go away on their own or are mild enough that they don't interfere with quality of life.
Lifestyle and home remedies
To reduce or relieve tremors:
- Avoid caffeine. Caffeine and other stimulants can increase tremors.
- Use alcohol sparingly, if at all. Some people notice that their tremors improve slightly after they drink alcohol, but drinking isn't a good solution. Tremors tend to worsen once the effects of alcohol wear off. Also, increasing amounts of alcohol eventually are needed to relieve tremors, which can lead to alcohol use disorder.
- Learn to relax. Stress and anxiety tend to make tremors worse. Being relaxed may improve tremors. You can't rid your life of all stress. But you can change how you react to stressful situations using a range of relaxation techniques, such as massage or meditation.
-
Make lifestyle changes. Use the hand less affected by tremor more often. Find ways to avoid writing with the hand affected by tremor, such as using online banking and debit cards instead of writing checks.
Try voice-activated commands on your smartphone and speech-recognition software on your computer.
Coping and support
For many people, essential tremor can have serious social and psychological consequences. If the effects of essential tremor make it difficult to live your life as fully as you once did, consider joining a support group.
Support groups aren't for everyone, but you might find it helpful to have the encouragement of people who understand what you're going through. Or see a counselor or social worker who can help you meet the challenges of living with essential tremor.
Preparing for an appointment
You'll likely start by seeing your primary care provider. Or you might be referred immediately to a doctor trained in brain and nervous system conditions, called a neurologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medications, vitamins or other supplements you take, including the doses.
- Questions to ask your health care provider.
Take a family member or friend along, if possible, to help you remember the information you're given.
For essential tremor, some questions to ask your health care provider include:
- What's the most likely cause of my symptoms?
- Are there other possible causes?
- What tests do I need?
- How does essential tremor usually progress?
- What treatments are available, and which do you recommend?
- I have other health conditions. How can I best manage these conditions together?
- Are there restrictions I need to follow?
- Should I see a specialist? If so, whom do you recommend?
- Are there brochures or other printed materials I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your care provider is likely to ask you a number of questions, such as:
- When did your symptoms begin?
- Do you have a family history of tremor?
- Have you ever had a head injury?
- What parts of your body are affected?
- Does anything make your tremors better or worse?



