Brain AVM (arteriovenous malformation)
Overview
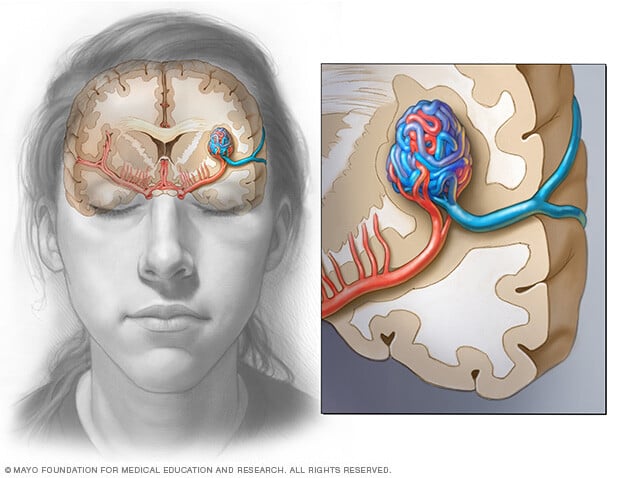
A brain arteriovenous malformation (AVM) is a tangle of blood vessels that creates irregular connections between arteries and veins in the brain.
Arteries take oxygen-rich blood from the heart to the brain. Veins carry oxygen-depleted blood back to the lungs and heart. A brain AVM disrupts this vital process.
An arteriovenous malformation can develop anywhere in the body, but common locations include the brain and spinal cord. Overall, brain AVMs are rare.
The cause of brain AVMs isn't clear. Most people who have them are born with them, but they can form later in life. Rarely, AVM can be a trait passed down in families.
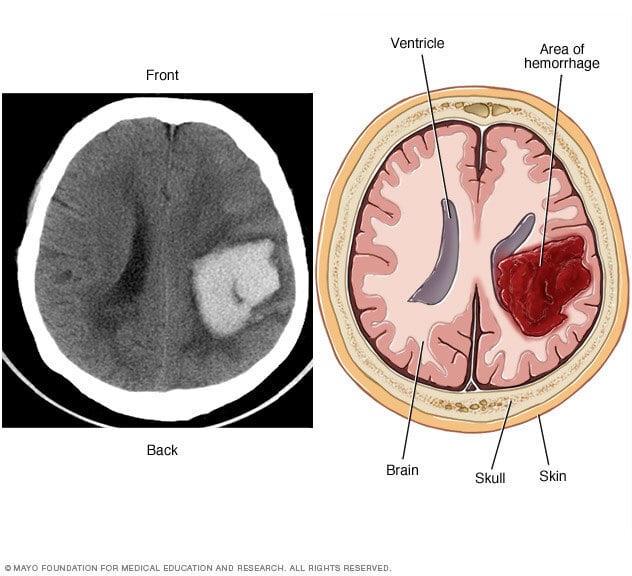
Some people with brain AVMs experience symptoms such as headaches or seizures. A brain AVM may be found after a brain scan for another health issue. Sometimes a brain AVM is found after the blood vessels burst and bleed, known as a hemorrhage.
Once diagnosed, a brain AVM can be treated to prevent complications such as brain damage or stroke.
Symptoms
A brain arteriovenous malformation (AVM) may not cause any symptoms until the AVM bursts and bleeds, known as a hemorrhage. In about half of all brain AVMs, a hemorrhage is the first sign of the malformation.
But some people with brain AVMs may experience symptoms other than bleeding, such as:
- Seizures.
- Headaches or pain in one area of the head.
- Muscle weakness or numbness in one part of the body.
Some people may experience more-serious symptoms depending on the location of the AVM, including:
- A very bad headache.
- Weakness, numbness or paralysis.
- Vision loss.
- Trouble speaking.
- Confusion or not being able to understand others.
- Trouble with walking.
Symptoms of a brain AVM may begin at any age but usually appear between ages 10 and 40. Brain AVMs can damage brain tissue over time. The effects slowly build and often cause symptoms in early adulthood.
By middle age, however, brain AVMs tend to remain stable and are less likely to cause symptoms.
When to see a doctor
Get medical care right away if you notice any symptoms of a brain AVM, such as seizures, headaches or other symptoms. A bleeding brain AVM is dangerous and requires emergency medical care.
Causes
The cause of brain arteriovenous malformations (AVMs) is not known. Researchers believe most brain AVMs are present at birth and form during a baby's growth in the womb. But brain AVMs can happen later in life as well.
Brain AVMs are seen in some people who have hereditary hemorrhagic telangiectasia (HHT). HHT also is known as Osler-Weber-Rendu syndrome. HHT affects the way blood vessels form in several areas of the body, including the brain.
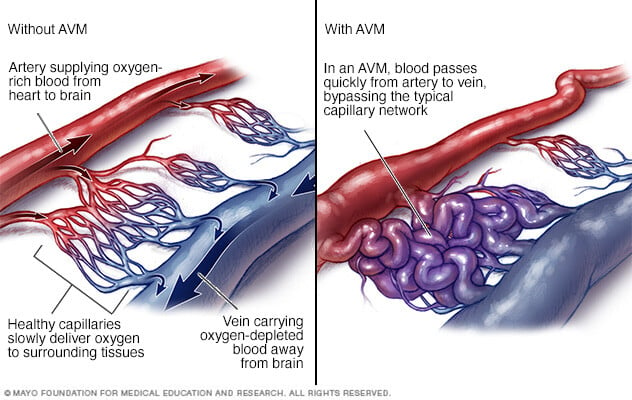
Typically, the heart sends oxygen-rich blood to the brain through arteries. The arteries slow blood flow by passing the blood through a series of smaller and smaller blood vessels. The smallest blood vessels are called capillaries. The capillaries slowly deliver oxygen through their thin, porous walls to the surrounding brain tissue.
The oxygen-depleted blood passes into small blood vessels and then into larger veins. The veins return the blood to the heart and lungs to get more oxygen.
The arteries and veins in an AVM lack this supporting network of smaller blood vessels and capillaries. Instead, blood flows quickly and directly from the arteries to the veins. When this happens, surrounding brain tissue doesn't receive the oxygen it needs.
Risk factors
Anyone can be born with a brain arteriovenous malformation (AVM), but these factors may raise the risk:
- Being male. Brain AVMs are more common in men.
- Having a family history. Rarely, brain AVMs occur in families, but it's not clear if there's a certain genetic risk factor. It's also possible to inherit other medical conditions that increase the risk of brain AVMs, such as hereditary hemorrhagic telangiectasia (HHT).
Complications
Complications of a brain arteriovenous malformation (AVM) include:
-
Bleeding in the brain. A brain AVM puts extreme pressure on the walls of the affected arteries and veins. The pressure causes the arteries and veins to become thin or weak. This may result in the AVM breaking open and bleeding into the brain, known as a hemorrhage.
This risk of a brain AVM bleeding ranges from around 2% to 3% each year. The risk of bleeding may be higher for certain types of AVM. Risk also may be higher in people who have had a brain AVM bleed in the past.
Although studies haven't found that pregnancy increases the risk of hemorrhage in people with a brain AVM, more research is needed.
Some hemorrhages associated with brain AVMs aren't detected because they cause no major symptoms. However, potentially dangerous bleeding can occur.
Brain AVMs account for about 2% of all hemorrhagic strokes each year. In children and young adults who experience brain hemorrhage, brain AVMs are often the cause.
-
Reduced oxygen to brain tissue. With a brain AVM, blood doesn't flow through the network of small blood vessels called capillaries. Instead, it flows directly from arteries to veins. Blood rushes quickly because it isn't slowed by the smaller blood vessels.
Surrounding brain tissue can't easily absorb oxygen from the fast-flowing blood. Without enough oxygen, brain tissues weaken or may die off completely. This results in stroke-like symptoms, such as trouble speaking, weakness, numbness, vision loss or trouble staying steady.
- Thin or weak blood vessels. An AVM puts extreme pressure on the thin and weak walls of the blood vessels. A bulge in a blood vessel wall, known as an aneurysm, may form. The aneurysm may be at risk of bursting.
-
Brain damage. The body may use more arteries to supply blood to the fast-flowing brain AVM. As a result, some AVMs may get bigger and displace or compress portions of the brain. This may prevent protective fluids from flowing freely around the brain.
If fluid builds up, it can push brain tissue against the skull.
One type of brain AVM that involves a major blood vessel called the vein of Galen causes serious complications in babies. Symptoms are present at birth or appear soon after birth. This type of brain AVM causes fluid to build up in the brain and the head to swell. Swollen veins may be seen on the scalp, and seizures may occur. Children with this type of brain AVM can have a failure to thrive and congestive heart failure.
Diagnosis

To diagnose a brain arteriovenous malformation (AVM), your healthcare professional reviews your symptoms and conducts a physical exam.
One or more tests may be used to diagnose brain AVM. Imaging tests are usually done by radiologists trained in brain and nervous system imaging, known as neuroradiologists.
Tests used to diagnose brain AVMs include:
-
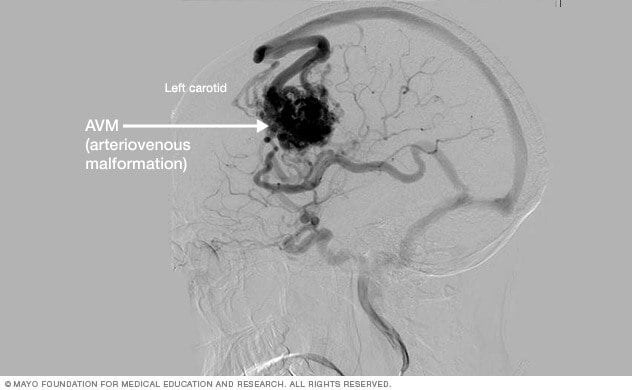
Cerebral angiography. This is the most detailed test to diagnose a brain AVM. Cerebral angiography reveals the location of the feeding arteries and draining veins, which is critical to planning treatment. Cerebral angiography is also known as cerebral arteriography.
In this test, a long, thin tube called a catheter is inserted into an artery in the groin or wrist. The catheter is threaded to the brain using X-ray imaging. A dye is injected into the blood vessels of the brain to make them visible under X-ray imaging.
-
Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create a detailed cross-sectional image of the brain.
Sometimes a dye is injected through a tube into a vein for the CT scan. This type of test is known as computerized tomography angiography. The dye allows the arteries feeding the AVM and the veins draining the AVM to be viewed in greater detail.
-
Magnetic resonance imaging (MRI). MRI uses powerful magnets and radio waves to create detailed images of the brain.
MRI is more sensitive than CT and can show subtle changes in brain tissue related to a brain AVM.
MRI also provides information about the exact location of the brain AVM and any related bleeding in the brain. The information is important for planning treatment.
A dye also may be injected to see the blood circulation in the brain. This type of test is known as magnetic resonance angiography.
Treatment
There are several treatments for brain arteriovenous malformation (AVM). The main goal of treatment is to prevent bleeding, known as a hemorrhage. Treatment also can help control seizures or other brain symptoms.
The proper treatment depends on your age, health, and the size and location of the brain AVM.
Medicines may be used to treat symptoms caused by the AVM, such as headaches or seizures.
Surgery is the most common treatment for brain AVMs. There are three surgical options:
-
Surgical removal, known as resection. Surgery may be recommended if the brain AVM has bled or is in an area that can easily be reached. In this procedure, the surgeon removes part of the skull to gain access to the AVM.
With the help of a high-powered microscope, the surgeon seals off the AVM with special clips and carefully removes it from surrounding brain tissue. The surgeon then reattaches the skull bone and closes the incision in the scalp.
Resection usually is done when the AVM can be removed with little risk of hemorrhage or seizure. AVMs that are in deep brain regions carry a higher risk of complications, and other treatments may be recommended.
-
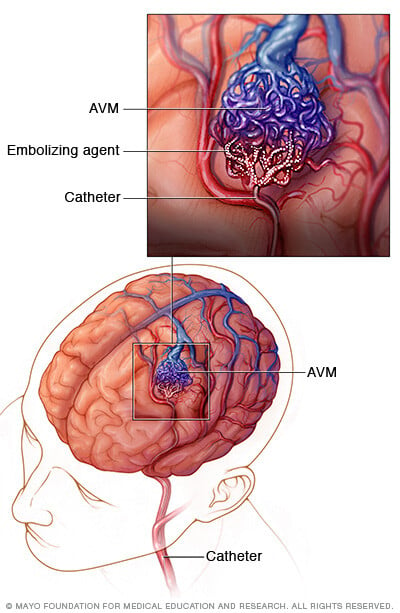
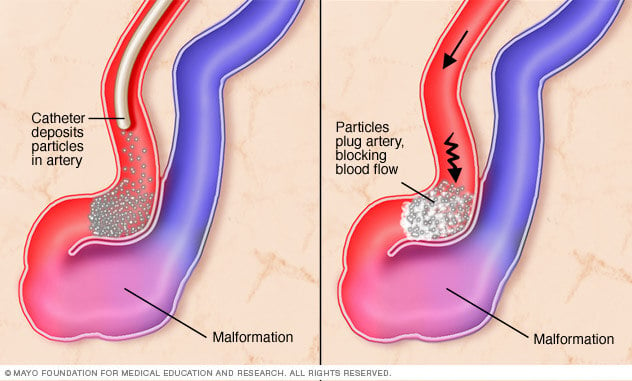
Endovascular embolization. In this procedure, a catheter is inserted into an artery in the leg or wrist. The catheter is threaded through blood vessels to the brain using X-ray imaging.
The catheter is positioned in one of the arteries that feeds the brain AVM. The surgeon injects an embolizing agent. This may be small particles, a gluelike substance, microcoils or other materials. The embolizing agent blocks the artery and reduces blood flow into the AVM.
Endovascular embolization is less invasive than traditional surgery. It may be performed alone but it's often used before other surgical treatments to make them safer. It does this by reducing the size of the brain AVM or the likelihood of bleeding.
In some large brain AVMs, endovascular embolization may be used to reduce stroke-like symptoms by redirecting blood back to brain tissue.
-
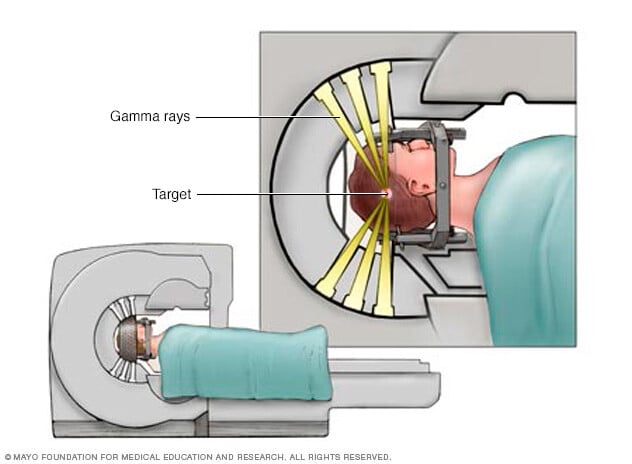
Stereotactic radiosurgery (SRS). This treatment uses precisely focused radiation to destroy the AVM. This type of surgery doesn't require cuts in the body the way other surgeries do.
Instead, SRS directs many highly targeted radiation beams at the AVM to damage the blood vessels and cause scarring. The scarred AVM blood vessels then slowly close in 1 to 3 years.
This treatment may be done for small AVMs that are hard to remove with traditional surgery. It also may be done for AVMs that haven't caused dangerous hemorrhages.
Sometimes healthcare professionals decide to monitor a brain AVM rather than treating it. This may be recommended if you have few or no symptoms or if your AVM is in an area of your brain that's hard to treat. Monitoring includes regular medical checkups with your healthcare team.
Potential future treatments
Researchers are studying ways to better predict the risk of hemorrhage in people with brain AVM. This can help better guide treatment decisions. For example, high blood pressure within the AVM and hereditary syndromes that affect the brain may affect the risk of hemorrhage.
Innovations in imaging technology also are being evaluated. Innovations include 3D imaging, brain tract mapping, and functional imaging, which produces images of blood flow to certain areas of the brain. The techniques have the potential to improve surgical precision and safety in removing brain AVMs and preserving surrounding blood vessels.
Ongoing advances in embolization, radiosurgery and microsurgery techniques also are making it possible to use surgery to treat brain AVMs that were hard to access in the past. Advances also are making it safer to remove brain AVMs during surgery.
Coping and support
You can take steps to cope with the emotions that may come with a diagnosis of brain arteriovenous malformation (AVM) and the recovery process. Consider trying to:
- Learn about brain AVM to make informed decisions about your care. Ask your healthcare professional about the size and location of your brain AVM. Ask how that affects your treatment options. As you learn more about brain AVMs, you may become more confident in making treatment decisions.
- Accept your emotions. Complications of brain AVM, such as hemorrhage and stroke, can cause emotional concerns as well as physical ones. Recognize that experiencing emotions is common. Some emotional and mood changes may be caused by the injury itself, along with coming to terms with the diagnosis.
- Keep friends and family close. Keeping your close relationships strong helps during recovery. Friends and family can provide the practical support you need, such as coming with you to healthcare appointments and providing emotional support.
- Find someone to talk with. Find a good listener who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or support group also may be helpful.
Ask your healthcare professional about support groups in your area. You also might look online or check the library. You may find a support group through a national organization, such as the American Stroke Association or the Aneurysm and AVM Foundation.
Preparing for an appointment
A brain arteriovenous malformation (AVM) may be diagnosed in an emergency right after bleeding has occurred. It also may be found after other symptoms prompt a brain scan.
But sometimes a brain AVM may be found during the diagnosis or treatment of an unrelated medical condition. You may then be referred to a specialist trained in brain and nervous system conditions, such as a neurologist or neurosurgeon.
Because there's often a lot to discuss, it's a good idea to arrive prepared for your appointment. Here are some tips to help you get ready and what to expect from your healthcare professional.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance.
- Write down any symptoms you're experiencing, including any that don't seem related to the reason for which you scheduled the appointment.
- Make a list of all medicines, vitamins and supplements that you're taking.
- Ask a family member or friend to come with you, if possible. Sometimes it can be hard to remember all the information provided to you during an appointment. Someone who comes with you may remember something that you forgot or missed.
- Write down questions to ask. Also, don't be afraid to ask questions that may come up during your appointment.
Your appointment time is limited, so preparing a list of questions ahead of time helps make the most of your time. For brain AVM, some basic questions to ask include:
- What are other possible causes of my symptoms?
- What tests will I need to confirm the diagnosis?
- What are my treatment options and the pluses and minuses for each?
- What results can I expect?
- What kind of follow-up should I expect?
What to expect from your doctor
Your neurologist is likely to ask about any symptoms you may be experiencing, do a physical exam and schedule tests to confirm the diagnosis.
The tests gather information about the size and location of the AVM to help direct your treatment options. Your neurologist may ask:
- When did your symptoms start?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
What you can do in the meantime
Avoid any activity that may raise your blood pressure and put stress on a brain AVM, such as heavy lifting or straining. Also avoid taking any blood-thinning medicines, such as warfarin (Jantovin).



