Seizures
Overview
A seizure is a sudden, uncontrolled burst of electrical activity in the brain. It can cause changes in behavior, movements, feelings and levels of consciousness. Having two or more seizures at least 24 hours apart that don't have a known cause is considered to be epilepsy.
There are many types of seizures, and they have a range of symptoms and severity. Seizure types vary by where they begin in the brain and how far they spread. Most seizures last from 30 seconds to two minutes. A seizure that lasts longer than five minutes is a medical emergency.
Seizures can happen after a stroke or a head injury. They also may be caused by an infection such as meningitis or another illness. Many times, though, the cause is unknown.
Most seizures can be controlled with medicine. However, managing seizures can affect your daily life. You can work with your health care professional to balance seizure control and medicine side effects.
Symptoms
Symptoms vary based on the type of seizure. They also can range from mild to severe. Seizure symptoms may include:
- Temporary confusion.
- A staring spell.
- Jerking movements of the arms and legs that can't be controlled.
- Loss of consciousness or awareness.
- Cognitive or emotional changes. They may include fear, anxiety or a feeling that you've already lived this moment, known as deja vu.
A classification system distinguishes the different types of seizures. Health care professionals typically classify seizures as focal or generalized. Seizures are classified based on how and where the brain activity causing the seizure began. If health care professionals don't know how the seizures began, they may classify the seizures as unknown onset.
Focal seizures
Focal seizures result from electrical activity in one area of the brain. This type of seizure can occur with or without loss of consciousness:
- Focal seizures with impaired awareness. These seizures involve a change or loss of consciousness or awareness that feels like being in a dream. People having these types of seizures may seem awake but they stare into space and don't respond to their environment. They may perform repetitive movements such as hand rubbing, mouth movements, repeating certain words or walking in circles. They may not remember the seizure or even know that it occurred.
-
Focal seizures without impaired awareness. These seizures may alter emotions. They also may change the way things look, smell, feel, taste or sound. But the seizures don't cause a loss of consciousness.
During these types of seizures, people may suddenly feel angry, joyful or sad. Some people have nausea or unusual feelings that are hard to describe. These seizures may result in trouble speaking and involuntary jerking of a body part such as an arm or a leg. They also may cause sudden sensory symptoms such as tingling, dizziness and seeing flashing lights.
Symptoms of focal seizures may be confused with other conditions of the brain or nervous system. They include migraine, narcolepsy or mental illness.
Generalized seizures
Seizures that appear to involve all areas of the brain from the time they start are called generalized seizures. Different types of generalized seizures include:
- Absence seizures. Absence seizures, formerly known as petit mal seizures, often occur in children. Absence seizures typically cause a person to stare into space or make subtle body movements such as eye blinking or lip smacking. They usually last for 5 to 10 seconds. These seizures may happen up to hundreds of times a day. They may occur in clusters and can cause a brief loss of awareness.
- Tonic seizures. Tonic seizures cause stiffening of the muscles. These seizures usually affect muscles in the back, arms and legs. People who experience these seizures may lose consciousness and fall to the ground.
- Atonic seizures. Atonic seizures, also known as drop seizures, cause a loss of muscle control. People having this type of seizure may suddenly fall down or drop their head.
- Clonic seizures. Clonic seizures are associated with repeated jerking muscle movements. These seizures usually affect the neck, face and arms on both sides of the body.
- Myoclonic seizures. Myoclonic seizures usually appear as sudden brief jerks or twitches of the arms and legs. There is often no loss of consciousness.
- Tonic-clonic seizures. Tonic-clonic seizures, previously known as grand mal seizures, are the most dramatic type of epileptic seizure. They can cause a sudden loss of consciousness, body stiffening and shaking. They sometimes cause people to lose control of their bladder or to bite their tongue. They may last for several minutes. Tonic-clonic seizures also may start as focal seizures that then spread to involve most or all of the brain.
Seizure stages
Seizures can have a beginning phase, middle phase and end phase.
-
Prodrome. This is the earliest warning that a seizure may occur, but it is not part of the seizure itself. During the prodrome, people may have a hard-to-describe sense that a seizure may happen. They also may have changes in behavior. This can happen in the hours or even days before a seizure.
The prodrome stage may include an aura. The aura is the first symptom of a seizure. Symptoms during the aura may include the feeling that a person or place is familiar, known as deja vu, or a feeling that a person or place is not familiar. Or people may simply feel strange, feel fear or panic, or even have pleasant feelings. Symptoms also may include smells, sounds, tastes, blurred vision or racing thoughts. The prodrome may include a headache, numbness or tingling, nausea, or dizziness.
Many people with seizures have a prodrome or aura as part of their experience, but some people do not.
- Ictal. The middle part of a seizure is called the ictal phase. The ictal phase spans the time from the first symptom to the end of the seizure. Symptoms of the ictal phase depend on the type of seizure.
-
Postictal. This is the period after a seizure during recovery. The postictal stage can last minutes or hours. Some people recover quickly while others take hours. The length of the postictal stage depends on the type of seizure and what part of the brain was affected.
During this phase, people may be slow to respond, have trouble with memory, and have trouble talking or writing. They may feel sleepy, confused, dizzy, sad, scared, anxious or frustrated. They also may have nausea, a headache, weakness, feel thirsty or have a loss of bladder control.
When to see a doctor
Seek immediate medical help if you have a seizure or if you see someone have a seizure and any of the following occurs:
- The seizure lasts more than five minutes.
- The person isn't breathing after the seizure stops.
- A second seizure follows immediately.
- The seizure is accompanied by a high fever.
- The seizure is accompanied by heat exhaustion.
- The person who had the seizure is pregnant.
- The person who had the seizure has diabetes.
- The seizure resulted in an injury.
If you experience a seizure for the first time, seek medical advice.
Causes
Nerve cells in the brain, known as neurons, create, send and receive electrical impulses. This allows the cells to communicate. Anything that disrupts the communication pathways can lead to a seizure. Some types of seizures may be caused by genetic changes.
The most common cause of seizures is epilepsy. But not every person who has a seizure has epilepsy. Sometimes seizures may be caused or triggered by:
- A high fever. When this happens, the seizure is known as a febrile seizure.
- An infection of the brain. This may include meningitis or encephalitis.
- Severe general illness, including a severe infection of COVID-19.
- Lack of sleep.
- Low blood sodium. This can happen with medicine that makes you urinate.
- Certain medicines that treat pain, depression or help people stop smoking. They can make it easier for seizures to happen.
- A new, active brain injury, such as head trauma. It can cause bleeding in an area of the brain or a new stroke.
- The use of legal or illegal drugs that may be sold on the streets, such as amphetamines or cocaine.
- Alcohol misuse, including during times of withdrawal or extreme intoxication.
Complications
Having a seizure can sometimes lead to complications that are dangerous for you or others. You might be at risk of:
- Falling. If you fall during a seizure, you can injure your head or break a bone.
- Drowning. If you have a seizure while swimming or bathing, you're at risk of accidental drowning.
- Car accidents. A seizure that causes loss of awareness or the inability to control a vehicle while conscious can be dangerous.
- Pregnancy complications. Seizures during pregnancy pose dangers to people who are pregnant and their babies. And certain anti-seizure medicines increase the risk of birth defects. If you have epilepsy and plan to become pregnant, work with your health care professional. Your care professional can adjust your medicines and monitor your pregnancy as needed.
- Mental health issues. People with seizures are more likely to have depression, anxiety or other emotional health issues. Dealing with the condition and the side effects of anti-seizure medicines can cause these issues.
Diagnosis
After a seizure, a health care professional thoroughly reviews your symptoms and medical history. You may need several tests to determine the cause of your seizure and evaluate how likely it is that you'll have another one.
Tests may include:
- A neurological exam. A health care professional may evaluate your behavior, motor abilities and mental function.
- Blood tests. You may need to give a blood sample to check your blood sugar levels and look for signs of infections or genetic conditions. You also may have the levels of salts in your body checked. These salts are known as electrolytes and control the balance of fluids.
- Lumbar puncture, known as a spinal tap. If an infection is suspected as the cause of a seizure, you may need to have a sample of cerebrospinal fluid removed for testing.
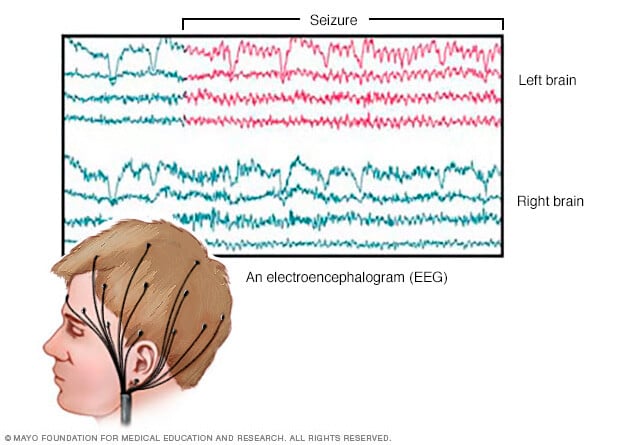
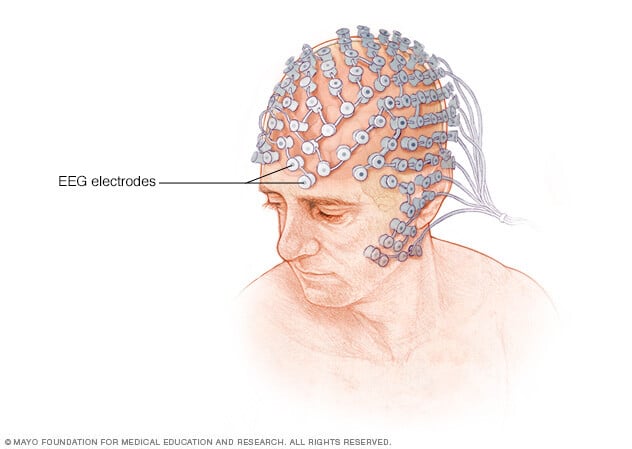
An electroencephalogram (EEG). In this test, electrodes attached to your scalp record the electrical activity of your brain. The electrical activity shows up as wavy lines on an EEG recording. The EEG may reveal a pattern that tells whether a seizure is likely to occur again.
EEG testing also may help exclude other conditions that mimic epilepsy. Depending on the details of your seizures, this test may be done at a clinic, overnight at home or over a few nights in the hospital.
Imaging tests may include:
- Magnetic resonance imaging (MRI). An MRI scan uses powerful magnets and radio waves to create a detailed view of your brain. An MRI may show changes in the brain that could lead to seizures.
- Computerized tomography (CT). A CT scan uses X-rays to obtain cross-sectional images of your brain. CT scans can reveal changes in your brain that might cause a seizure. Those changes may include tumors, bleeding and cysts.
- Positron emission tomography (PET). A PET scan uses a small amount of low-dose radioactive material that's injected into a vein. The material helps reveal active areas of the brain and detect changes.
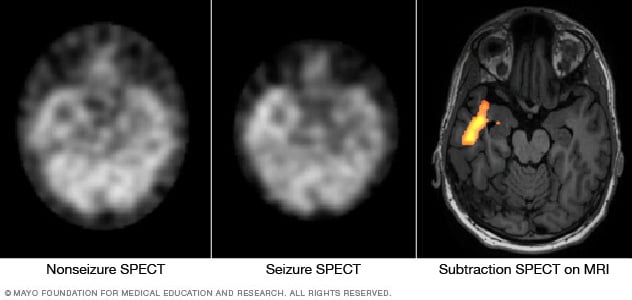
Single-photon emission computed tomography (SPECT). A SPECT test uses a small amount of low-dose radioactive material that's injected into a vein. The test creates a detailed 3D map of the blood flow in your brain that happens during a seizure.
A health care professional also may conduct a type of SPECT test called subtraction ictal SPECT coregistered to MRI (SISCOM). The test may provide even more-detailed results. This test is usually done in a hospital with overnight EEG recording.
Treatment

Not everyone who has one seizure will have another one. Because a seizure can be an isolated incident, you may not need to start treatment unless you've had more than one.
The optimal goal in seizure treatment is to find the best possible therapy to stop seizures, with the fewest side effects.
Medications
Treatment of seizures often involves the use of anti-seizure medicines. There are many different options for anti-seizure medicines. Most people with epilepsy will stop having seizures after trying just one or two medicines.
The goal of medicine is to find what works best for you and causes the fewest side effects. Sometimes a health care professional might recommend more than one medicine.
Finding the right medicine and dosage can be complex. You may need to try several different medicines. Common side effects may include weight changes, dizziness, fatigue and mood changes. Very rarely, more-serious side effects can cause damage to the liver or bone marrow.
A health care professional considers your condition, how often you have seizures, your age and other factors when choosing which medicine to prescribe. The care professional also will review any other medicines you may be taking to ensure that the anti-seizure medicines won't interact with them.
Dietary therapy
Following a ketogenic diet can improve seizure control. A ketogenic diet is high in fat and very low in carbohydrates. But it can be challenging to follow because there's a limited range of foods allowed.
Variations on a high-fat, low-carbohydrate diet also may be helpful but less effective. They include low glycemic index and Atkins diets. These modified diets are still being studied.
Surgery
If treatment with at least two anti-seizure medicines isn't effective, surgery may be an option. The goal of surgery is to stop seizures from happening. Surgery works best for people who have seizures that always begin in the same place in the brain. There are several types of surgery, including:
- Lobectomy. Surgeons locate and remove the area of your brain where seizures begin.
- Thermal ablation, also called laser interstitial thermal therapy. This less invasive procedure focuses highly concentrated energy at a specific target in the brain where seizures begin. This destroys the brain cells that cause seizures.
- Multiple subpial transection. This type of surgery involves making several cuts in areas of the brain to prevent seizures. It's usually done when the area of the brain where seizures start can't be safely removed.
- Corpus callosotomy. This surgery cuts the network of connections between the neurons of the right and left halves of the brain. This is used to treat seizures that start in one half of the brain and travel to the other half. However, even after surgery, seizures may still occur on the side of the brain where they started.
- Hemispherotomy. This surgery completely disconnects one side of the brain from the rest of the brain and body. This type of surgery is only used when medicines aren't effective in managing seizures and when seizures affect only half the brain. Many daily functional abilities may be lost after this surgery. But children can often recover those abilities with rehabilitation.
Electrical stimulation
If the area of the brain where seizures start is unable to be removed or disconnected, devices that provide electrical stimulation may help. They can reduce seizures along with continued anti-seizure medicine use. Stimulation devices that may offer seizure relief include:
- Vagus nerve stimulation. A device implanted underneath the skin of the chest stimulates the vagus nerve in the neck, sending signals to the brain that inhibit seizures.
- Responsive neurostimulation. A device is implanted on the surface of the brain or within brain tissue. The device can detect seizure activity and deliver electrical stimulation to stop the seizure.
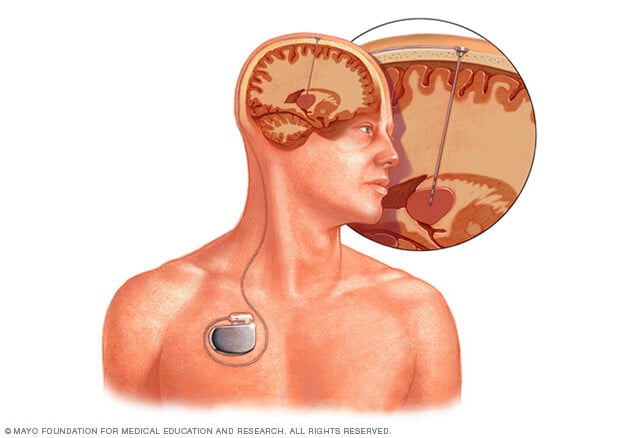
- Deep brain stimulation. Surgeons implant thin wires called electrodes within certain areas of the brain to produce electrical impulses. The impulses regulate the brain activity that causes seizures. The electrodes attach to a pacemaker-like device placed under the skin of the chest. This controls the amount of stimulation produced.
Pregnancy and seizures
Women who've had seizures typically are able to have healthy pregnancies. But birth defects related to certain medicines can sometimes occur.
In particular, valproic acid — a medicine for generalized seizures — has been associated with cognitive deficits and neural tube defects, such as spina bifida, in babies. The American Academy of Neurology recommends that women don't use valproic acid during pregnancy because of risks to their babies.
Discuss these risks with your health care team. Creating a plan with your health care team before you become pregnant is particularly important. In addition to the risk of birth defects, pregnancy can alter your medicine levels.
In some cases, it may be appropriate to change the dose of seizure medicine before or during pregnancy. The goal is to be on the lowest dose of the safest seizure medicine that is effective for seizure control.
Taking folic acid before pregnancy may help prevent some complications related to taking anti-seizure medicines while pregnant. Folic acid is found in standard prenatal vitamins. It's recommended that all people of childbearing age take folic acid while on anti-seizure medicines.
Birth control and anti-seizure medicines
Some anti-seizure medicines can alter the effectiveness of birth control. Ask your health care professional if your medicine may interact with your birth control. Other forms of birth control may need to be considered.
Potential future treatments
Researchers are studying other potential therapies to treat seizures. They include therapies to stimulate the vagus nerve, other cranial nerves or the brain without surgery.
One area of research showing promise is MRI-guided focused ultrasound. The therapy involves pointing ultrasound beams, which are sound waves, to an area of the brain that's causing the seizures. The beam creates acoustic energy to destroy brain tissue in a targeted way without surgery. This type of therapy can reach deeper brain structures. It also can focus on a target without damaging the nearby tissue.
Lifestyle and home remedies
Here are some steps you can take to help with seizure control:
- Take medicine correctly. Don't adjust the dosage before talking to your health care professional. If you feel that your medicine should be changed, talk about it with your care professional.
- Get enough sleep. Lack of sleep can trigger seizures. Be sure to get adequate rest every night.
- Wear a medical alert bracelet. This will help emergency personnel know how to treat you correctly if you have another seizure.
- Be active. Exercising and being active may help keep you physically healthy and reduce depression. Make sure to drink enough water and rest if you get tired during exercise.
- Make healthy life choices. Managing stress, limiting alcohol and not smoking all factor into a healthy lifestyle.
Treatment
Personal safety
Seizures don't usually result in serious injury, but if you have recurrent seizures, injury is a possibility. These steps can help you avoid injury during a seizure:
- Take care near water. Don't swim alone or ride in a boat without someone nearby.
- Wear a helmet for protection during activities such as bike riding or sports participation.
- Take showers instead of baths unless someone is near you.
- Modify your furnishings. Pad sharp corners, buy furniture with rounded edges and choose chairs that have arms to keep you from falling off of them. Consider carpet with thick padding to protect you if you do fall.
- Display seizure first-aid tips in a place where people can easily see them. Include any important phone numbers.
- Consider a seizure detection device. The Food and Drug Administration has cleared a watch-like prescription device that can detect tonic-clonic seizures (Embrace2). The device alerts loved ones or caregivers so that they can check on you and ensure your safety. Talk with your health care professional to decide if using this type of device might be appropriate for you.
Lifestyle and home remedies
Seizure first aid
It's helpful to know what to do if you witness someone having a seizure. If you're at risk of having seizures in the future, pass this information along to family, friends and co-workers so that they know what to do if you have a seizure.
To help someone during a seizure, take these steps:
- Carefully roll the person onto one side.
- Place something soft under the person's head.
- Loosen tight neckwear.
- Don't put your fingers or other objects in the person's mouth.
- Don't try to restrain someone having a seizure.
- Clear away dangerous objects if the person is moving.
- Stay with the person until medical help arrives.
- Observe the person closely so that you can provide details on what happened.
- Time the seizure.
- Stay calm.
Coping and support
Stress due to living with a seizure disorder can affect your mental health. It's important to talk with your health care provider about your feelings and seek ways you can find help.
At home
Your family members can provide much-needed support. Tell them what you know about your seizures. Let them know they can ask you questions, and be open to conversations about their worries. Help them understand your condition by sharing educational materials or other resources that your health care professional has given you.
At work
Meet with your supervisor and talk about your seizures and how they affect you. Discuss what you need from your supervisor or co-workers if a seizure happens while at work. Consider talking with your co-workers about seizures. This will help widen your support system and bring about acceptance and understanding.
You're not alone
Remember, you don't have to go it alone. Reach out to family and friends. Ask your health care professional about local support groups or join an online support community. Don't be afraid to ask for help. Having a strong support system is important to living with any medical condition.
Preparing for an appointment
Sometimes seizures need immediate medical attention, and there's not always time to prepare for an appointment.
Other times, your first appointment to evaluate a seizure may be with your health care professional. Or you may be referred to a specialist. You might see a specialist trained in brain and nervous system conditions, known as a neurologist. Or you might be referred to a neurologist trained in epilepsy, known as an epileptologist.
To prepare for your appointment, consider what you can do to get ready. Also understand what to expect.
What you can do
- Record information about the seizure. Include the time, location, symptoms you experienced and how long it lasted, if you know these details. Seek input from anyone who may have seen the seizure, such as a family member, friend or co-worker. They might provide information you may not know.
- Be aware of any pre-appointment restrictions. At the time you make the appointment, ask if there's anything you need to do in advance to be ready for any medical tests or exams.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking, including dosages.
- Take a family member or friend along to help you remember all the information provided during an appointment. Because you may not be aware of everything that happens when you're having a seizure, someone who was a witness can provide helpful information.
- Write down questions to ask. Preparing a list of questions will help you make the most of your time during your visit.
For seizures, some basic questions to ask your health care professional include:
- What do you think caused my seizure?
- Do I need to have any tests done?
- What treatment approach do you recommend?
- What are the alternatives to the primary approach that you're suggesting?
- How likely is it that I might have another seizure?
- How can I make sure that I don't hurt myself if I have another seizure?
- I have these other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask any other questions you may have during your appointment and anytime that you don't understand something.
What to expect from your doctor
A health care professional is likely to ask you a number of questions:
- Can you describe your seizure episode?
- Where were you and what happened right before it started?
- Was anyone there to witness what happened?
- What do you remember feeling just before the seizure? What about right after the seizure?
- What symptoms did you experience?
- How long did the seizure last?
- Have you ever had a seizure or other neurological issue in the past?
- Do you have any family members who have been diagnosed with a seizures or epilepsy?
- Have you recently traveled outside the country?