Pain medicines after surgery
It's natural to have concerns about the pain you might have after surgery. It's also natural to be concerned about the possible risks of taking powerful pain medicines. Controlling pain and lowering the risk of side effects are important for your comfort, recovery and rehabilitation after surgery.
It's best to talk about pain relief and pain medicines before you have surgery. Being prepared can help you better manage your pain.
Planning for surgery
Before surgery, you'll likely speak with your surgeon or other members of your healthcare team. You may discuss pain management, treatment options and your particular needs. You might talk about your:
- Pain expectations. Ask about pain that typically is associated with the surgery. Also ask about how long your recovery may last.
- Previous experiences with pain. Talk to your healthcare team about your experience with pain and methods of pain control. Mention what has and hasn't worked for you in the past.
- Chronic pain. If you take medicines to treat chronic pain, list your daily medicine usage and your typical pain levels. Discuss options with your healthcare team for treating both chronic pain and pain relating to your surgery.
- List of your medicines. Give your healthcare team a list of all your prescription medicines and medicines that you take without a prescription. Also include any supplements or herbs you've taken in the past month. Members of your healthcare team need to know about anything that might interact with the medicines you take for pain after surgery. You may need to change your medicines before and after surgery.
- Alcohol and drug use. Accurately describe your current use of alcohol, tobacco or illicit drugs. Your healthcare team needs to know if you are recovering or currently have alcohol use disorder or if you use illicit drugs. Also tell your healthcare team if you misuse prescription medicines. The information helps your healthcare team plan and monitor your pain management.
- History of medicine misuse. If you have misused medicines in the past, it is important to share this with your healthcare team. It's also important for your healthcare team to know if you take medicines used for addiction, such as naltrexone or suboxone.
- Concerns about side effects. Ask for written information about the pain medicines you may be prescribed after surgery and their side effects. Ask about what can be done to decrease side effects and when to get help for serious side effects.
- Pain management without medicines. Ask about ways to support your treatment plan without medicines, such as getting counseling to address anxiety or coping skills.
- Other concerns. Let your healthcare team know about any other concerns, including if you're worried about overdosing on pain medicines. They can help you understand strategies to safely manage your pain.
Types of pain medicine
Pain after surgery usually is managed with more than one pain medicine, also known as an analgesic. The right type, delivery and dose of medicines for you depend on the type of surgery and expected recovery, as well as your own needs.
Pain medicines include the following:
- Opioids, powerful pain medicines that lower the perception of pain, may be given after surgery. Intravenous opioids may include fentanyl, hydromorphone, morphine, oxycodone, oxymorphone and tramadol. Examples of opioids prescribed in pill form after surgery include oxycodone (OxyContin, Roxicodone, others) and oxycodone with acetaminophen (Percocet).
- Local anesthetics are medicines that numb a part of your body. They cause a short-term loss of feeling in that part of the body. These medicines include lidocaine and bupivacaine.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) lessen the swelling that worsens pain. NSAIDs that may be taken after surgery include ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve), celecoxib (Celebrex, Elyxyb) or ketorolac.
- Other nonopioid pain relievers include acetaminophen (Tylenol, others) and ketamine (Ketalar).
- Other medicines that can treat pain after surgery include the anti-anxiety medicine midazolam and the anti-seizure medicines gabapentin (Gralise, Horizant, Neurontin) and pregabalin (Lyrica).
Opioids may or may not be appropriate to use after your surgery. Your surgeon will likely prescribe a combination of treatments. These may help control pain and lessen side effects. A combination of treatments also can help you resume activity appropriate for recovery and lower the risks associated with opioids.
Managing the risks of opioid use
Opioids are often critical for managing pain after surgery because of their powerful effect. But they can have side effects, including nausea, vomiting, constipation, urinary retention, drowsiness, impaired thinking skills and trouble breathing.
Overdosing and misuse of opioids also are risks, especially when opioids are used to treat ongoing pain, known as chronic pain. Although the use of opioids after surgery is intended as a short-term strategy to relieve pain while the body heals, the risk of misuse is still a concern.
Because of the risks, use these medicines carefully, if at all. To lower the risks, take opioids at the smallest dose that is effective for the shortest possible time.
Talk to your healthcare professional about steps you can take to lower the risks associated with opioids, including:
- Taking medicines only as directed, and taking the smallest effective dose for the shortest amount of time.
- Telling your healthcare professional when your pain is not under control.
- Not drinking alcohol while taking opioids.
- Following your healthcare team's instructions about other medicines not to take while using opioids.
- Storing medicines safely.
- Disposing of unused medicines, ideally through a pharmacy take-back program.
- Not sharing your medicine with other people.
Pain relief after major surgery

A primary goal of pain management after major surgery is for you to awaken relatively comfortable and to transition to pain control. However, some discomfort is common and should be expected after surgery.
Intravenous (IV) pain medicine. Before surgery, you'll likely have a slender plastic tube called a catheter inserted into a vein in your hand or arm. The catheter allows your healthcare team to give you fluids, sedatives, anesthetics, antibiotics or pain medicines. The catheter can be used for delivering pain medicines until you can take pills by mouth.
Pain relievers, such as opioids, are usually injected into your IV catheter at regular intervals. Most hospitals also offer patient-controlled analgesia (PCA). PCA is a system that allows you to give yourself a fixed dose of the medicine by pushing a button. This way you don't have to ask a nurse for each dose of pain medicine.
The PCA system has built-in safeguards to prevent you from overdosing on pain medicine. If you push the button more than once within a set period of time, the dispenser ignores the second request.
- Wound infiltration anesthesia. Your surgeon may inject an anesthetic drug at the wound site during the surgery. Or your surgeon may place a catheter to deliver pain medicines after surgery. This may reduce the use of opioids during your recovery.
Spinal anesthesia. Some surgeries can be done with spinal anesthesia, which involves medicines injected directly into the spinal fluid.
Spinal anesthesia is easier and faster than epidural analgesia. But it doesn't last as long because there's no catheter to allow the delivery of more medicine if needed. A long-acting opioid may be added to the spinal medicine to relieve pain for up to 24 hours.
Nerve block. A nerve block uses a local anesthetic to provide targeted pain relief to an area of your body, such as an arm or leg. It prevents pain messages from traveling up the nerve pathway to your brain. Nerve blocks can be used for outpatient procedures or more-involved inpatient surgery.
For pain relief lasting several hours, an injection is used for a nerve block. For longer pain control, a catheter may be inserted for continuous medicine delivery or patient-controlled delivery.
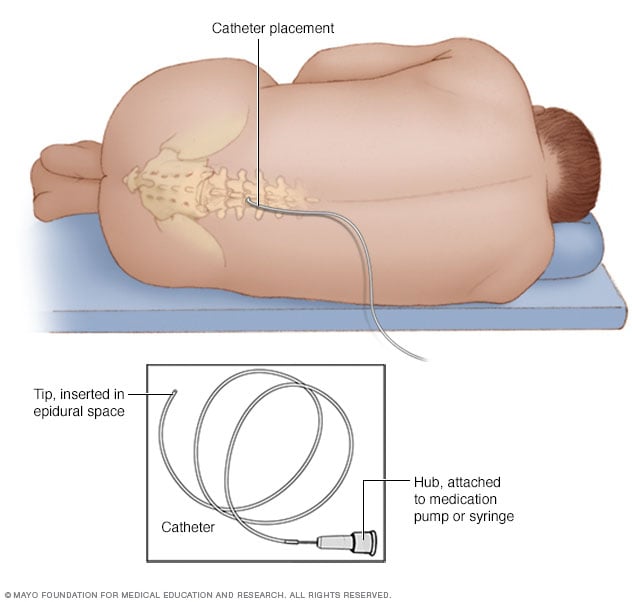
Epidural analgesia. Pain medicines are injected through a catheter inserted into the epidural space within your spinal canal but outside your spinal fluid. An epidural catheter is often used for labor and delivery. It sometimes is used before an operation, such as a cesarean section or major abdominal surgery.
The epidural catheter can be left in place for several days if needed to control pain after surgery. A continuous infusion of pain relievers, including local anesthetics or opioid medicines, can be delivered through the catheter to control pain.
Patient-controlled epidural analgesia (PCEA), similar to PCA, enables you to give yourself a dose of the pain medicine by pushing a button. It, too, has built-in safeguards so that you don't give yourself too much medicine.
Pain relief after minor surgery and during home recovery
After surgery, you're given instructions for general care. This may include rest, applying ice packs, doing rehabilitative exercises and caring for your wound. Ask to have written instructions to bring home with you.
These instructions may be the main way you relieve pain after minor surgery. If you've had major surgery, the instructions help with a more comfortable transition off medicine.
You will likely switch to oral pain medicines before leaving the hospital. You might continue to take them at home to manage pain. You may take a combination of medicines in pill form, which may include:
- Opioids.
- Acetaminophen (Tylenol, others).
- NSAIDs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
Be sure you know what active ingredient is in each pain medicine, what the appropriate dose is and how often to take it. Also ask your healthcare team about possible interactions with other medicines. These include cold medicine that you buy from the store, other prescription medicines and supplements.
Your role in pain control
After surgery, work with your healthcare team to make your recovery as quick and pain-free as possible. Communicate with members of your healthcare team to help them assess and adjust the pain management plan.
- Be honest about the pain you feel after surgery. Let your healthcare professional know how much it hurts, where it hurts, and what activities or positions make it better or worse. Rate the intensity of pain on a 0 to 10 scale, where 0 is no pain and 10 is the worst pain you can imagine. The more specific you can be, the better your healthcare team can help you.
- Don't ignore side effects. Tell your care team if you experience sleepiness, constipation, nausea or other side effects of the medicines. A different pain medicine or dose can sometimes reduce uncomfortable side effects, and these side effects can often be treated and relieved.



